Active surveillance pioneer calls for end to transrectal biopsies--ASAP.
Where will the American Urological Association guidelines panel stand?
By Howard Wolinsky
The death knell for the transrectal biopsy may have sounded on Saturday afternoon at the popular Prostate Cancer Research Institute’s Patient Conference. Or at least, it should have.
Laurence Klotz, MD, one of the founders of Active Surveillance (AS) and a powerful voice in urology, rang the bell for change—transrectal biopsies should be phased out. STAT.
(Laurence Klotz, MD, of the University of Toronto, gives thumbs up to patient advocacy.)
Mark Moyad, MD, of the University of Michigan, was the moderator of this part of the PCRI patient program.
Klotz, a once-aspiring jazz musician, opened by playing and singing Paul Simon’s “Still Crazy After All These Years” on a grand piano in his home in Toronto.
But in his statements in favor of transperineal biopsy, he sounded far from crazy to me.
Moyad asked Klotz his thoughts about transrectal biopsies vs. the safer transperineal biopsies, a hotly debated topic among prostate cancer patients on active surveillance and also among urologists in the U.S.
Klotz supported transperineal (TP) biopsies, in which biopsy cores are taken through the area between the anus and the scrotum. TP avoids the germy rectum used in transrectal, or transfecal, biopsies that can introduce bacteria into the sterile prostate gland and cause potentially deadly and disabling sepsis.
I have asked Klotz about this topic in the past. He told me he was equally deft with either technique in terms of cancer detection and the infection rate.
But this was the first time I heard him say he has only performed transperineal biopsies in recent years.
This statement seemed to catch Moyad off guard
“Why were transperineals – I’m asking this out of sheer lack of knowledge – not being done 15 years ago?” he asked.
I can answer that. They were. But the technology was different and patients had to be put under general anesthesia, which poses issues of its own for elderly patients and their ability to tolerate general anesthesia, and also TPs ties up precious OR time.
Transrectal biopsies didn’t become a bread-and-butter procedure for urologists until the late 1980s with the introduction of biopsy guns, ultrasound guidance, and prostate-specific antigen (PSA) blood testing.
In recent years, new technology has been introduced to enable urologists to perform transperineal biopsies in their offices using only local anesthesia.
Klotz gave Moyad his take on why transrectal biopsies still are the mainstay in the U.S.
”First of all, never underestimate the power of inertia in established practice in sustaining a certain practice. Second, the transrectal biopsy is easier. The prostate is right there. It’s technically an easy procedure, less demanding in terms of time and anesthesia.
“I think the patients do have more pain doing a transperineal. It’s quite easy to get effective anesthesia with the transrectal. It can be a real challenge doing it transperineally. Some people do it in the operating room. We just simply don’t have the resources so I do it under local.”
Patients who have had both procedures confirm that the TP can be slightly more painful but tolerable with brief pain as the local anesthesia takes hold.
Klotz continued: “Another reason for resistance to change was the way it was done initially was in the operating room. People want to operate in the operating room. They don’t want to use that precious time to do something like a biopsy. Finally, most patients do well.”
Klotz noted the sepsis rate from the transrectal biopsy is in the 2-4% range. “Ninety-five plus percent of patients sail through it. You need the kind of rare events, some of which can be catastrophic, to drive change,” he said.
As key opinion leaders such as Klotz throw their weight behind transperineal biopsies, new problems will arise.
Only 5% of the 2 million prostate biopsies performed each year in the U.S. are done transperineally. So overnight change will be difficult though even the American Urological Association has been hosting TP training sessions at its meetings.
AUA in 2017 endorsed transrectal biopsies in its guidelines with a mention of old-style transperineal biopsies performed with steppers and templates as a secondary choice.
Outside the U.S., there is a movement away from transrectal biopsies.
The dangers of transrectal biopsies became front-page news in Norway in 2019. Oslo hair stylist Agnes Gulbrandsen forced the issue when her father died from a brain embolism triggered by sepsis. Researcher Truls Bjerklund Johansen confirmed that a biopsy he performed on Roar Gulbrandsen was the cause of the sepsis.
Klotz recounted the story, which I have covered in detail. Overnight, Norwegian men voted with their feet and prostates and pressured urologists to switch to transperineal biopsies.
(Watch Dr. Bjerklund Johansen and Agnes Gulbrandsen in a video I organized for ASPI. Go to August 2021 at https://aspatients.org/meeting-videos/)
(Agnes Gulbrandsen led a campaign to stop transrectal biopsies in Norway that has become an international effort.)
(Agnes and her late dad Roar, who died from a brain embolism triggered by sepsis.)
Bjerklund Johansen estimates that 2,000 American men a year experience death by transrectal biopsy—a claim that American urologists have greeted with disbelief. The researcher stands by his numbers.
In January 2021, the European Association of Urologists (EAU) made the transperineal prostate the preferred biopsy in Europe to protect patients from death by biopsy from sepsis as well as to prevent other infections.
Urologist Heinrich Van Poppel, policy head of the EAU, told me in a recent interview that transrectal biopsies are now considered “malpractice” in Europe.
Van Poppel said the EAU’s position basically comes down to protecting patient safety and concern about microbial resistance caused by overuse of antibiotics in transrectal biopsies. The Europeans favor antibiotic stewardship.
Many, if not most, urologists here steadfastly defend transrectal biopsies as the “gold standard,” denying Bjerklund Johansen’s inconvenient research and resisting migration to transperineal biopsies.
Doctors complain about lost time and expense in learning the transperineal technique. Many assume their sepsis rates are low—without really looking at them.
Why are the American docs in denial? They don’t know what they don’t know. So they may not want to review their infection rates. It costs $40,000 plus taking out time for some training to get on the transperineal train. Some urologists may want to keep doing what they’re doing.
In “No More Men Need to Die From Transrectal Prostate Biopsies—A movement toward transperineal biopsies” I wrote last year in MedPageToday: “The old maxim holds that doctors bury their mistakes. In the case of deaths by transrectal biopsies, mistakes often may be buried under a misleading cause listed on death certificates. Doctors don't often link deaths from septic shock to transrectal biopsies performed a few days earlier.”
Urinary tract infection makes it on the death certificate. But no one explores the likely cause of the infection—a transrectal biopsy.
(Death by TRUS biopsy was front-page news in Norway in 2019. Will it be in the U.S?)
Compared with surgery, a transrectal biopsy may seem like a harmless option. It isn't. The rectal lining is with potentially infectious bacteria, and 5 to 7 percent of patients who undergo prostate biopsies — the vast majority of which are transrectal — develop infections, according to the American Urological Association. In up to 3 percent of transrectal biopsy cases, the infections trigger potentially life-threatening and disabling sepsis.
Some critics have told me I may be overboard and unrealistic about adoption of transperineal biopsies. They say some poorly trained doctors may adopt transperineal as a marketing ploy to attract patients.
So as always, buyer beware.
Meanwhile, this is the time for patient action:
—Consider a safer transperineal biopsy if your doctor recommends a biopsy. Transperineal biopsies can be hard to come by in the U.S. Have a transrectal if that’s the only practical option.
—As with any procedure, try to find doctors with a lot of experience.
—Ask your urologist for their infection rates with transrectal vs. transperineal biopsies. It’s extremely rare, but TPs can sometimes be linked to infections.
—Ask your doctors if and when they plan to switch to transperineal biopsies. Let your wishes be known. A Canadian radiation oncologist told me medicine is like any other business, and doctors won’t consider change unless we let them know our preferences.
—If you don’t like the answers, shop in your community or beyond for a urologist.
—Sign my petition at Change.org calling on transrectal biopsies to be phased out.
I have asked Klotz to sign it and join Van Poppel and even a past president of the American Urological Association and hundreds of patients who support change. When it hits 1,000 signatures, we can circulate it to Congress, Medicare, and the AUA.
Meanwhile, the AUA has begun work on revising its guidelines on biopsies. New guidelines will be released in 2023. I’m not holding my breath.
On which side of history will the AUA guidelines committee stand? On the side of the status quo? Or the side of patient safety?
Don’t miss: ASPI (Active Surveillance Patients International) will be premiering the first of a new video series titled “Active Surveillance 101" at noon Eastern on September 24, 2022.
Register here: ASPI SEPTEMBER ZOOM MEETING
Like 101-level courses in colleges, AS 101 is aimed at teaching the basics. In this case, it's the basics of active surveillance, close monitoring of low- to favorable intermediate-risk prostate cancer.
The program features conversations between actual patients and their partners/spouses and leading experts. The goal of this series is to reach all AS candidates, including those who have not yet been diagnosed with prostate cancer but have rising PSAs (prostate-specific antigen) blood levels and offer them an introduction to AS and help them formulate questions when they go to their family doctors, urologists, or oncologists.
The first episode features a couple, Nancy and Larry White in a simulated office visit with Dr. Steve Spann, a top family physician and dean of the University of Houston College of Medicine. They discuss Larry's rising PSA and what it may mean.
In subsequent episodes, the couple visits Dr. Laurence Klotz, of the University of Toronto, the "father of active surveillance." Other episodes of AS 101 are being developed on biopsies, imaging, and DNA testing.
AS 101 is sponsored by the Active Surveillance Coalition, which includes Active Surveillance Patients International, the AnCan Virtual Support Group for Active Surveillance, Prostate Cancer Support Canada, Prostate Cancer Research Institute, and TheActiveSurveillor.com newsletter. We encourage you to share this series with anyone you know who is dealing with this issue, including your family physician.
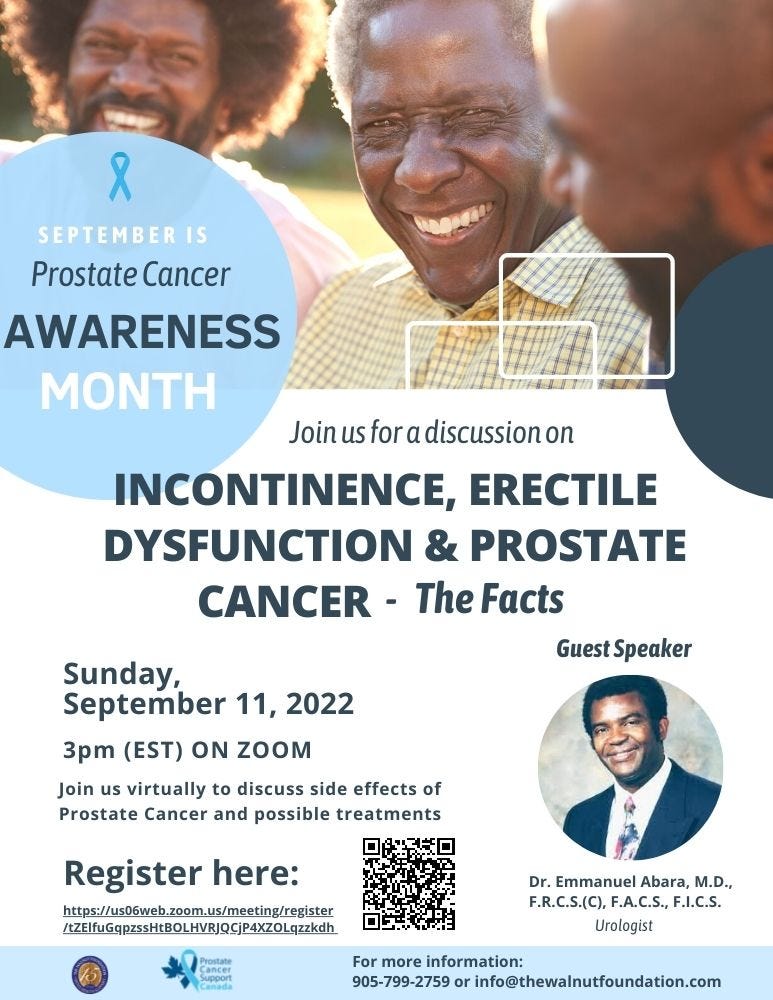
The Walnut Foundation Monthly Meeting in support of Prostate Cancer Awareness Month.
Topic:-Incontinence, Erectile Dysfunction & Prostate Cancer with Special Guest. Dr. Emmanuel Abara, Urologist.
This is a free webinar. You may submit your questions in advance to info@thewalnutfoundation.com
Prostate Cancer Support Canada meets virtually. Yanks are welcome.
The Prostate Cancer Support Canada is holding its 2022 Prostate Cancer Virtual Conference September 17-18 in honor of Awareness Month.
Day 1, The ‘New Normal’ for Support Groups, will focus on facilitation and communication skills for those in, or interested in, leadership roles in the prostate cancer support community.
Day 2, Prostate Cancer Realities will more broadly address issues of interest to our community including managing anxiety and stress throughout the cancer journey, genetics and prostate cancer, upcoming research, how to find trusted information about prostate cancer, and more.
Dr. Brian Goldman, best-selling author and host of White Coat, Black Art on CBC radio, will be speaking about The ‘New Normal’ for Support Groups.
Check for details in the conference program ‘flipbook’ with session + speaker details and registration link: https://bit.ly/2022PCVCprogram
Prostate Cancer Foundation is looking at physical and mental illness.
For Prostate Cancer Awareness Month, the Prostate Cancer Foundation, the 800-pound private prostate cancer researcher, is holding a webinar on “Physical and Mental Wellness in Prostate Cancer.”
Here are the details:
Join us for the first in a series of monthly webinars hosted by PCF President and CEO Dr. Charles J. Ryan.
During Prostate Cancer Awareness Month, PCF challenges everyone to Get Healthy. Dr. Ryan and guests will discuss key aspects of nutrition, exercise, and mental health in prostate cancer.
The event will be Sept. 20, 2022 04:30 PM in Pacific Time (US and Canada).
Sign up to join here.
Following each segment, there will be a live Q&A.
• Prostate 8: Simple lifestyle changes that work (Dr. Stacey Kenfield, UCSF)
Dr. Kenfield is Associate Professor in the Department of Urology and is the Helen Diller Family Professor of Population Science for Urologic Cancer. She is an expert on lifestyle, exercise, nutrition, and their impact on prostate cancer. She'll discuss research showing how specific lifestyle factors improve outcomes after prostate cancer diagnosis, and practical ways to incorporate these changes into your life.
• Mental Health and Prostate Cancer (Dr. Andrew Roth, Memorial Sloan Kettering Cancer Center)
Dr. Roth is an Attending Psychiatrist and is board-certified in Psychiatry, Geriatric Psychiatry, and Psychosomatic Medicine. He is focused on caring for the mental health needs of patients with prostate cancer and other genitourinary diseases. He'll provide an overview of the challenges patients commonly face, as well as strategies and resources for coping and living well during treatment and survivorship.
Here’s hoping Dr. Roth will cover AS as well as advanced prostate cancer.
Please send any questions for the speakers in advance to: webinar@pcf.org







Might want to relook at your message below.
RBeach. I read it over three times and can't pinpoint the sentence and sentences to which you are referring. Happy to correct. But can you point out the offending sentence or sentences. I appreciate the help. HW