An overdose of overdiagnosis: Aussie urologist takes on the debate on whether low-risk prostate 'cancer' actually is cancer
Recording of Dr. Jonathan Epstein's webinar available--don't miss it. Taking a Biden break.
(Editor’s note: Dr. Jeremy Grummet is a urology leader and reformer from Down Under. He has led the charge against transrectal biopsies in favor of safer transperineal biopsies through the TRexit group. He was a guidelines panelist for the European Association of Urologists, which in 2021 made transperineal biopsies the preferred biopsy in Europe and Australia. He’s an academic urologist at Monash University and Director of Urology at Alfred Health in Melbourne.
(Jeremey shares his thoughts on urology and beyond in his Substack newsletter Vermiculations. The word “vermiculations” has various definitions, including track marks from a worm, bodily functions, and wavelike muscle contractions of the alimentary tract that moves food along.
(With Dr. Grummet’s permission, I reprint his newsletter on whether low-risk prostate “cancer” is actually a cancer. Check out Vermiculations.—Howard Wolinsky)
By Dr. Jeremy Grummet
Low-grade prostate cancer might look like cancer down a microscope, but it doesn’t behave like cancer. Understanding prostate cancer overdiagnosis is critical for patients and clinicians navigating men’s health challenges in modern urology.
The overview effect is what astronauts experience when they gaze at Earth from space. Not a borderline to be seen. The petty details of humanity and its too-often sordid history erased by the view from their distant orbital perspective. A sense of awe and an overwhelming desire to protect our planet emerges. This perspective shift is vital for healthcare professionals seeking holistic patient care in medicine.
(Dr. Jeremy Grummet)
As surgeons, we must pay attention to detail. Our patients’ lives can depend on it, especially in prostate cancer treatment. But we can also get stuck in the weeds, unable to see the wood for the trees, or get distracted by decoys in clinical practice. Focusing solely on microscopic findings risks missing the bigger picture of patient outcomes.
We’re dazzled, for example, by the flurry of new robotic surgery technologies.
Innovations in minimally invasive surgery and robotic prostatectomy promise precision, but do they always improve quality of life? And we get wowed by the survival benefit of adding even more hormone-based therapy, with all its morbid side effects, for metastatic prostate cancer. These advancements in oncology and cancer treatment captivate us, yet hormone therapy side effects can burden patients unnecessarily. We can be too close, sometimes, to see the bigger picture of evidence-based medicine.
But if we zoom out, what might appear in our field of vision that makes patient-centered care possible? Exploring prostate cancer screening, active surveillance, and personalized medicine could reveal paths to avoid overtreatment and prioritize wellness. By addressing healthcare costs, embracing shared decision-making, and leveraging medical research, we can redefine cancer care for better long-term outcomes.
The EAU25 conference in Madrid [in March], but a pattern emerged there which has stuck with me since. In every prostate cancer session, it seemed, was the unrelenting concern about overdiagnosis in early detection. Overdiagnosis in ERSPC, overdiagnosis in ProBase, overdiagnosis in ProScreen. You might say we were overdosing on overdiagnosis.
But what exactly is this overdiagnosis we are all so worried about? It’s the detection of ISUP Grade Group 1, or Gleason 6 cancer in the old language. We call it overdiagnosis because we know that this form of prostate cancer is itself harmless, apart from the anxiety it causes patients and because still too many patients with it are unnecessarily treated We say that we would prefer to not detect it at all because of its indolent nature. (Yet, illogically, when we do detect it, we follow these patients closely on active surveillance – work that out!)
We know from the most rigorous studies in PSA testing that screening of men aged 50-70 with PSA on a repeated basis can reduce death from prostate cancer (9). Too often ignored is also screening’s ability to reduce prostate cancer metastasis (and its morbid systemic treatment), at a rate around double that of its mortality reduction. ERSPC showed that this occurs even prior to MRI being introduced to the diagnostic algorithm.
MRI has now been standard of care in the diagnostic process for prostate cancer for several years, as recommended in the EAU Guidelines. By using it to triage for biopsy, it can avoid up to half of all biopsies – the main source of detection of GG1 disease, i.e. of overdiagnosis. But still we worry about overdiagnosis! And as a result, the argument remains against prostate cancer screening due to harms apparently outweighing benefits.
And let’s not kid ourselves, the benefits of treatment when we do detect prostate cancer early are nowhere near as good as we’d like to think. For example, according to Vickers’ paper last year using statistical modelling to contemporize raw data from the SPCG-4 and PIVOT trials, we would have to operate on 30-50 patients with GG2 prostate cancer to prevent a single death from the disease. The vast majority of GG2 patients we treat with standard radical therapy (surgery or radiation), therefore, do not enjoy a mortality benefit. But this is an argument for surveillance, or in the near future, focal therapy, for such patients. It is not an argument against screening.
If the true argument against screening is overdiagnosis of GG1 disease as the harm that tips the scales away from the demonstrated benefit, then the simplest and most far-reaching way of avoiding overdiagnosis is to stop calling GG1 cancer. Overdiagnosis problem: solved!
Eggener and others have been urging this for years now but have been stonewalled by our pathologist colleagues who have as yet been unable to see past their microscopes to the human beings beyond. We can duly acknowledge their protests that GG1 does indeed have features consistent with a cancer, and at the same time argue philosophically for the greater good of still not labelling it as cancer. This is the greater good not only for the patient whose biopsy is on the slide, but for all future patients who stand to benefit from the rollout of risk-adapted screening programs.
Remember how we used to get hung up on ASAP or HG-PIN? Nowadays we ignore these and rightly so. With MRI now enabling us to target lesions, what may have been diagnosed as GG1 in the past era of systematic-only biopsies, is now more likely to be detected as GG2. MRI-targeted biopsy is therefore causing a grade shift. For this reason, we are now rightly offering active surveillance not only to GG1 patients, but to many with GG2 disease also.
From a clinical perspective, the GG1 of today is the HG-PIN of the past. It is time, therefore, for the sake of realizing the benefits of screening without the blight of overdiagnosis, for GG1 to be relabelled as non-cancer. We must continue to engage with and respectfully lobby our pathologist colleagues to consider making this positive change together.
As the EU and Australia move away from current opportunistic testing for prostate cancer with its inherent health inequities that disadvantage the less health-literate in our communities, and we edge towards planning risk-adapted screening, removal of this remaining impediment will only accelerate screening’s implementation.
Prostate cancer screening can then finally and rightfully sit alongside the well-established screening programs for the other common cancers such as cervix, breast and bowel. One day, as we sit back on our commercial spaceflight in contemplation, we may wonder how we could ever have practiced without it.
Join the Epstein follow-up webinar on May 31
By Howard Wolinsky
Dr. Jonathan Epstein, the noted uropathologist, is coming back to The Active Surveillor webinar audience for a one-hour Q&A starting at noon Eastern May 31.
Here’s your invitation:
When: May 31, 2025 noon Eastern (US and Canada)
Register in advance for this meeting:
https://us02web.zoom.us/meeting/register/sazI-npeR3OdGWyRIrVRYg
Send any questions to The Active Surveillor: Howard.wolinsky@gmail.com
Meanwhile, the video of Dr. Jonathan Epstein’s webinar for The Active Surveillor on May 17 has posted in The Active Surveillor’s YouTube channel:
Many kudos came in on the program, where Dr. Epstein told us about Active Surveillance, cribriform and loads more. You can view the recording here
While you’re there, check out other videos posted in The Active Surveillor’s YouTube Channel. Please like and subscribe
Still time to sign up for biopsy webinar May 24 at noon Eastern
The Biopsy Debate:
The Latest Updates on
Transperineal vs. Transrectal Biopsies
The debate over transperineal vs. transrectal biopsies continues. Four randomized trials in the past year alone have yielded contradictory results.
Active Surveillance Patients International’s monthly webinar will be focused on these issues with researcher Sanoj Punnen, MD, Professor of Urologic Oncology at the University of Miami, joining us as our featured speaker.
The program will be Saturday, May 24, from noon to 1:30 pm Eastern.
Register: https://zoom.us/meeting/register/UZVDHmq9Rlyw6y_mqmK0hg#/registration
Dr. Punnen is Vice Chair of Research, Desai Sethi Urology Institute, and Co-Chair of Genitourinary Site Disease Group, Sylvester Comprehensive Cancer Center, University of Miami Leonard M. Miller School of Medicine.
Dr. Punnen’s research interest is in prostate cancer, primarily related to imaging, genomic, and molecular biomarkers in the detection, risk stratification, and monitoring of prostate cancer. He is the lead investigator on two prospective clinical trials validating a novel blood-based biomarker called the 4KScore test for predicting the risk of clinically significant prostate cancer and the need for biopsy of the prostate. He is also the Principal Investigator on an ongoing NCI-funded prospective clinical trial examining the impact of prostate MRI and tissue-based genomic prognostic signatures in men undergoing Active Surveillance for prostate cancer.
Please send questions in advance to: contactus@aspatients.org
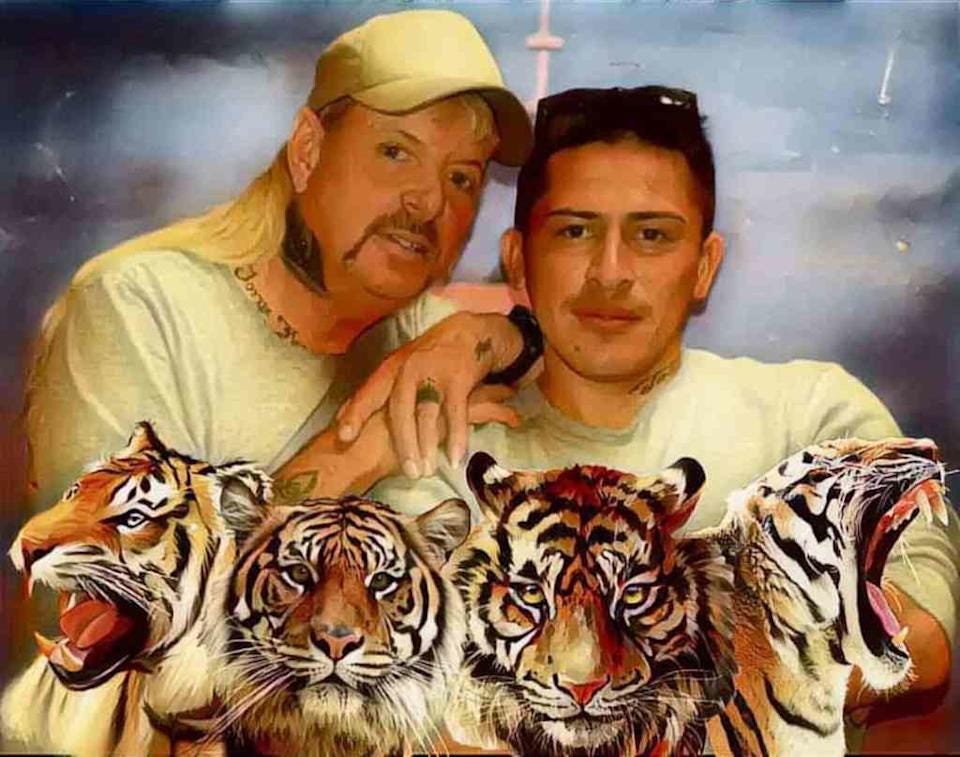
’Exotic Joe’: He has found love behind bars and his prostate cancer is back
By Howard Wolinsky
The last time we heard from Tiger King ex-Netflix star Joe Exotic [Joseph Maldonado], he was biding his time a in prison cell begging for a pardon from the President.
Joe, who engineered a seedy murder-for-hire plot to kill a rival zookeeper—AND now his prostate cancer is back and spread to his lungs.
Joe spoke to Radar Online from behind bars and shared updates. The 62-year-old is still serving a 21-year prison sentence for the murder-for-hire plot. While behind bars, he complained about his deteriorating health and eventually was diagnosed with prostate cancer.
Last year, his cancer went into remission after a year of chemotherapy and radiation.
Now he tells Radar Online :“The prostate cancer is back out of remission; the lung cancer is there now.”
While he previously predicted he would die in 2020, he shared that now his doctors feel confident that he can live with his cancer for many years. He doesn’t plan to seek further treatment and wants to ride things out until he can get released from prison, whether that’s through a presidential pardon or some other miracle.
“All of the doctors on the outside I’ve talked to said I can make it another 10 or 15 years without it killing me,” Joe explained. “And I really want to wait until I get out and get some real doctors with some class-act medical care and take care of it then.”
He has married fellow inmate Jorge Marquez, and the two had planned to move to Cozumel, Mexico, after his release. But Marquez is dealing with deportation problems.
Wow. The world is a zoo and a circus.
.







"Remember how we used to get hung up on ASAP or HG-PIN? Nowadays we ignore these and rightly so." The NCCN and AUA guidelines do not recommend ignoring ASAP. Atypical Small Acinar Proliferation means the cells don't look completely normal, but don't look like cancer. It's like being in a "gray zone." NCCN considers ASAP an indication for repeat biopsy within 3-6 months, resampling the site of ASAP and adjacent areas. AUA acknowledges ASAP as a high-risk finding requiring follow-up with a repeat biopsy within 3-12 months. NCCN views ASAP as a finding that warrants further investigation due to the increased likelihood of finding prostate cancer on a subsequent biopsy.
Best yet "Wow. The world is a zoo and circus."
I'd make a comment about the monkeys and the clowns, but I'd just get in trouble.