Bye-bye 'finger wave'? More MRIs before biopsies? Movember consensus recommends sweeping changes to AS protocols
U.S. community AS practice lags a decade behind UK and US academic practice
By Howard Wolinsky
Is it time to wave goodbye to the digital rectal exam--the so-called “finger wave”--and also time to say hello to more mpMRIs before performing biopsies on patients on active surveillance (AS) for low-risk prostate cancer?
An international consensus panel of health professionals and patients hosted by Movember, the men’s health charity based in Melbourne, Australia, makes these points and many more about changing the way AS patients should be monitored.
Movember commissioned the panel to help determine where it should allocate its research investments.
European Urology Oncology published online the consensus panel recommendations and avenues for research on AS.
The panel recommends sweeping changes in urology practice. It urges the demise of digital rectal exams--which presumably would put a coffin nail in all the jokes--as well as radical changes with greater use of mpMRIs and decreased use of biopsies.
Caroline Moore, MF FRCS (Urol), professor of urology at University College London, who led the work, said these protocols are common in the United Kingdom but less so internationally, including the United States.
Moore said protocols in the U.S. put many low-risk patients on AS “who may well have remained undiagnosed if they had been in the UK, as many men with a negative MRI don’t get a biopsy unless they have other worrying features. This means more men are able to avoid the risks from biopsies, such as discomfort and infections.”
“One of the striking things for me [in the consensus report] was seeing honestly that the UK is in a much better position than the U.S. as a whole for surveillance and diagnosis. The use of MRI before a biopsy is standard of care in NHS England. But I think internationally, it's important to remember that not everybody's in the place that we in the UK are in and that consensus meetings like this can help. That's the intent,” she said.
(Dr. Caroline Moore)
Moore, chief investigator of the Precision trial that in 2018 demonstrated the benefit of MRIs in diagnosing prostate cancer, said, “The United States, outside of academic centers, lags behind in adoption of these standards, compared to the UK.”
She said AS in some areas in the U.S. may lag a decade behind the UK.
Leonard Marks, MD, a urologist at David Geffen School of Medicine, UCLA, defended academic urology in the U.S., but agreed that community practice tends to lag behind in the U.S. in general.
Kevin Ginsburg, MD, a urologic oncologist at Wayne State University in Detroit, said he doesn’t view this as an academic vs. private practice issue but rather a difference in screening approaches and philosophy between the U.S. and the UK and the rest of Europe.
(Kevin Ginsburg, MD, Wayne State U., Detroit)
“European screening practices are very different in the UK vs. the U.S. In the UK, men with an elevated PSA routinely get an MRI. If that MRI is negative, men will not get a biopsy. This avoids diagnosis of many low-risk cancers, potentially at the cost of missing a few intermediate (IR) and high-risk (HR) cancers,” said Ginsburg, co-director of the MUSIC (Michigan Urological Surgery Improvement Collaborative), which leads the country in putting low-risk patients on AS with a 91% rate.
The rate of low-risk patients who opt to go on AS overall in the U.S. was 60% in 2021 compared with 94% in Sweden.
“In the U.S., we use MRI to target and mitigate some of the sampling error of a standard systematic biopsy, but men with a negative MRI in the U.S. still get a biopsy. This leads to the diagnosis of more low-risk cancers. Ultimately, it's a difference in philosophy. Would you avoid diagnosing many LR prostate cancers at the cost of missing a few IR and high-risk (HR) disease, or would you rather diagnose many/all IR/HR cancers at the cost of overdiagnosis and finding a lot of LR disease.”
That philosophical difference has a huge impact on patients like us. It can result in the overuse of transrectal biopsies, which carries risks, such as potentially disabling and deadly sepsis and other infections.
Moore contrasts the 6% of all patients diagnosed with cancer in the UK being low-risk with 33% in the U.S. The difference can be attributed to how MRIs are used. This suggests that many more of American patients go on AS with all that monitoring than need to be.
Research suggests that incorporating MRI in population-based prostate cancer screening decreases biopsy procedures with no difference in the detection of higher-grade cancer. American Urological Association and European Association of Urology guidelines incorporate mpMRI in the detection of prostate cancer and management for men enrolled in active surveillance.
But some centers maintain mpMRI should not replace periodic surveillance biopsies on active surveillance.
The consensus panel concluded that when patients have “stable parameters (PSA kinetics and density), consideration can be given to omitting routine biopsy, with discussion between the clinician and the patient.”
The panel also said digital rectal exams (DREs) can be omitted when MRI is used routinely in AS.
The demise of the DRE would represent a major change to urology practice and training.
It would be a culture changer, too. What would we do without all the jokes?
Digital rectal exams, the subject of countless jokes, patient complaints and embarrassment, have long been a standard feature of prostate exams in urology offices in the U.S. This exam is the first taught to urologists in training. Doctors feel for abnormalities of the gland, such as abnormal lumps or hard areas to screen for early signs of prostate cancer.
Jokes like this: “My doctor says it’s perfectly normal to get an erection during a prostate exam in fact he said, he already had one.” Bada boom.
Check out “urologist” Danny DeVito giving a digital rectal exam, to “patients” Michael Douglas: https://9gag.com/gag/aerE79B
And so on.
Some guys resist digital exams. Some straight men consider DREs bordering on a homosexual act. Seriously. I’ve heard this. Some men say the exam is painful.
Let’s face it. DREs just have a bad rap, are a pain in the ass, and don’t add much to the search for prostate cancer.
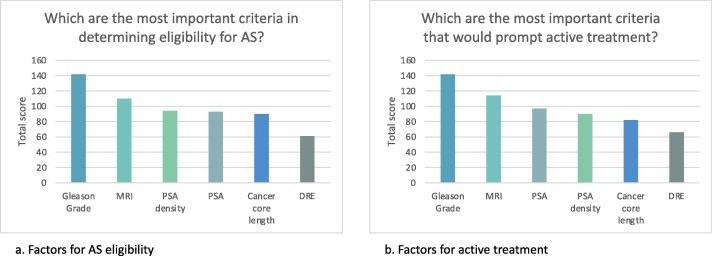
The panel added: “The use of DRE ranked lowest for both determining eligibility for and continuation on AS, due to its poor positive predictive value and impact on the patient. In fact, the use of DRE to initiate either additional tests (such as biopsy or MRI) or a treatment choice scored lowest among all tests, including PSA density, which is not commonly included in any of the guidelines.”
Guidelines from the American Academy of Family Physicians do not recommend family physicians perform DREs routine screening with prostate exams.
But the 2022 early detection guidelines from the American Urological Association recommend PSAs be performed not more frequently than every six months and for “updating a symptom assessment and physical examination with DRE every one to two years.”
In her practice in London, Moore said, “With our active surveillance program, we don't do digital rectal examination, and we don't do routine biopsies. We do biopsies as needed.”
Ginsburg said, “I do not do DRE on AS unless patients specifically request it. I am very, very, very comfortable replacing DRE with MRI. We have not published this data yet, but in MUSIC, in men on AS, DRE change is noted in less than 1% of men.”
Vincent J Gnanapragasam, MBBS BMedSci MA PhD FRCS FRCSEd(Urol), professor of urology at the University of Cambridge, said his group has not performed DRE for AS for probably eight to 10 years.
But UCLA’s Marks is not ready to abandon the finger wave.
He said: “Digital rectal exam should continue, in my opinion, not only for detection of the occasional prostate abnormality on palpation but also for detection of rectal lesions. Patients expect and appreciate the thoroughness of the exam. If not urologists, who will do this exam?”
(Leonard Marks, MD, David Geffen School of Medicine, UCLA.)
Moore stressed the need internationally for further research on personalized risk-adjusted dynamic active surveillance.
Fit the AS to the individual.
The panel said, ”The most important priority for research, across both the LE (lived experience) and the HCP (health care and research professionals) panels is the development of a personalized, dynamic, risk-adapted approach according to an agreed framework, with less testing in men at the lowest risk of progression. This risk-adapted approach contrasts with the current guideline-approved standardized approach.”
The panel added: “This represents a fundamental break with guideline-based practice in AS, not just in terms of practice, but in terms of the philosophy of care as well. As such, this priority calls for a major program of research, and Movember has set out a funding call to address this.”
Personally, starting at age 63, I was on a strict AS protocol starting in 2010 with annual biopsies for six years.
This was considered an advance over watchful waiting (WW), mainly aimed at much older men, a type of benign neglect that unfortunately resulted in many deaths.
Active surveillance in the late ‘90s was proposed to replace WW, which critics said entailed too much waiting and not enough watching.
We’ve seen in recent years mpMRIs have been added to protocols as a precursor biopsies.
Personally, I had my last biopsy and MRI almost seven years ago. But my 80+ cores in six biopsies only showed a tiny amount of cancer in a single core in 2010.
Now, I am followed with an annual PHI (Prostate Health Index), a type of PSA that includes regular PSA and free PSA and other data. My readings have been stable for years.
So my urologist came up with a different approach--not full AS and not full WW. Somewhere in-between.
I call it passive-aggressive surveillance. I am being surveilled with an annual PHI test, but no MRIs and biopsies unless needed.
If my PHI rises. it would trigger an MRI. If the PIRADS score is high, I’d have a biopsy. (Make mine transperineal, please.)
But your situation is likely different from mine. Hence, the need to personalize our protocols.
The panel agreed that “clinician confidence in AS, time to explain all the options, and the person or team informing patients of their diagnosis increase the likelihood of a choice of AS.”
I attend a really good AS support group in the UK. Several men there have noted sheepishly that they were put on AS by a nurse during COVID-19 three years ago and have yet to see a physician. Maybe that’s OK. But that seemed surprising to me.
(So the UK may not be a utopia either. Read The New Yorker about the “shattered” National Health Service, which is greatly stressed now.)
There was consensus in the LE (patient) panel that no upper age limit (such as 75 or 80 years old) should be applied, and there was uncertainty regarding a lower age limit. The HCP [health care and research professionals] panel was uncertain about an upper age limit but agreed that there should be no lower age limit for AS.
Patient age is a difficult topic. What age should you stop AS? I know one guy in his early 80s who wants off the AS merry-go-round because he feels his time on AS ought to be about done. I know another guy in his mid-80s, who wants to stay on AS into his 90s and beyond.
The report highlights this: “There was also uncertainty and disagreement in the LE panel about whether life expectancy (e.g., 10 or 15 years) should be used as an eligibility criterion. Discussion centered on the need to offer a full set of choices to men depending on their likelihood of benefitting from treatment, avoiding artificial barriers based on biological age or estimated life expectancy, which can lead to age discrimination. The HCP panel agreed that life expectancy of equal to or more than 10 years should be considered within the eligibility criteria for AS, with a shorter life expectancy requirement for intermediate-risk prostate cancer.”
The panel agreed that Gleason grade and MRI findings were the most important criteria in determining who should go on AS, with PSA density and PSA being the next most important ones.
The report noted: “There was much discussion on the use of other parameters, including cancer core length (in millimeters), tumor visibility, and tumor volume on MRI, none of which are recognized in established guidelines. There was agreement that percentage cancer in a biopsy core is a flawed concept as it does not consistently reflect absolute tumor volume and that numbers of positive cores should not be considered indicative of tumor burden in the context of MRI-targeted biopsies.”
It’s individualized. You need a protocol suited for you and your preferences,
The panel covered the concept of “surveillance fatigue,” where men and their families become tired of the process and the uncertainty of surveillance, and choose active treatment despite the stability of objective disease parameters.
Routine biopsies in surveillance increase surveillance fatigue, as does patient difficulty in accessing communication with their healthcare teams.
The consensus panel said more needs to be done to offer patients on AS psychological support.
“Men who are suitable for AS but experience, or are at risk of significant psychological consequences of AS, should be offered additional support rather than immediate active treatment,” the panel said.
The consensus report mentions the need to address the high dropout rate from AS excluding patients whose cancers have progressed but who leave because of AS “fatigue”, emotional distress, and other reasons.
Research suggests that up to 50% of patients on active surveillance for prostate cancer will discontinue their monitoring within five years. But there is little research on the reasons they do.
A 2022 Australian survey of 103 patients found that some of the most common reasons given by patients for discontinuing active surveillance included medical reasons such as disease progression and doctor recommendations, and personal reasons, such as anxiety and depression, inability to cope with uncertainty, desire to act, pressure from others such as spouses, inconvenience of the protocol, and fear of cancer progression.
Many of the participants who either received or considered treatment noted that they had weighed medical and personal factors equally in making their decision. 52% opted for definitive treatment.
In 2018, British researchers found in a study of 255 patients that the dropout rate at five years was 42% but it could be decreased to 22% with patients attending a single educational seminar.
The consensus paper states: “An MRI-led AS program, with no routine biopsies, showed dropout rates at 5 years in the absence of progression at less than one percent highlighting that education, support, and a more acceptable surveillance schedule all have an impact.”
The paper “acknowledged that the inclusion of routine biopsies in surveillance increases surveillance fatigue, as does difficulty in accessing communication with the health care team .”
Moore said in her panel of over 1,000 men on an MRI-led active surveillance program at University College London Hospitals Trust, the dropout rate when the disease is stable is rare, with fewer than 1% of men dropping out when the disease is stable over the past 15 years.
Marks said, “Counseling is everything. Already, the 'psychological consequences' of AS are diminishing, as knowledge of safety disseminates.”
The panel also urged urologists managing patients with AS not to routinely ask whether patients want to undergo more aggressive treatment, which can trigger emotional distress.
Gnanapragasam said, “We never do this. I’m mystified that this needs addressing.”
The panel did not address DNA testing, which is common practice in the U.S. but not in Canada or Europe.
This is surprising from an American POV.
Moore explained: “Essentially, both genomic-, tissue-, serum- and urine-based biomarkers don’t yet have a clear role in selecting men for AS, and more work is needed to see if they may do so in the future. I would say that Europe is rightly awaiting evidence of the usefulness of the tests when MRI is available.”
(Disclosure: I was a panel member and co-author of the paper as a representative of the AnCan Virtual Support Group for AS and as editor of TheActiveSurveillor.com. Other North American representatives came from Active Surveillance Patients International (Joe Gallo and Mark Lichty), Prostate Cancer Support Canada (Phil Segal), the Walnut Foundation (Anthony Henry), and ZERO—The End of Prostate Cancer (Jim Schraidt). Gallo and Schraidt also are. active in AnCan.
Funny thing. North American patients nearly didn’t serve on the panel. I heard about the conference from a meeting in UK and I asked if North American patients could attend. Movember graciously agreed to include us.
Repelling the ‘Invasion of the Prostate Snatchers’
As of Sunday, we have more than 800 registrants for the AnCan program on Monday evening featuring Dr. Mark Scholz, author of the groundbreaking book “Invasion of the Prostate Snatchers.”
The AnCan program is on at 8 p.m. Eastern, Monday, Jan. 30.
To register, click https://bit.ly/3Xf4nbm If you can’t attend, you can register and get a link to view the program at your convenience.
Scholz’s program, which I will co-moderate with AnCan’s Peter Kafka, is entitled, "Invasion of the Prostate Snatchers: The return 13 years later. An evening with Dr. Mark Scholz."
Registration for session is already a record-breaker.
But I have been reassured we have plenty of room.
Personally, I am a huge fan of Scholz. He and his patient/co-author Ralph Blum’s book helped me weather the gray zone of a rising PSA and an inconclusive biopsy. I had done all my homework, thanks to Scholz and Blum, by the time I finally was diagnosed with a microscopic Gleason 6 in a single core (never seen again) and was ready to go on active surveillance in December 2010.
The program is aimed at patients with the full spectrum of prostate cancer, from low-risk Gleason 6 to advanced cancers.
If you have any questions, you can send them to me at howard.wolinsky@gmail.com






My concern with the reliance on the MRI is the accuracy of the reading and interpretation. Inaccurate reading causes inaccurate decisions.
Dr. Charles Metzger from my friends at the Prostate Forum said this about the Movember consensus panel recommendations in the email edition of TheActiveSurveillor: "DRE was the only thing we had before PSA…what a sad state of affairs that was. PSA really changed the whole process especially using the density and free psa.
I do however agree with Dr Marks.
Although DRE didn’t help much in my practice for diagnosing prostate cancer I found all kinds of pathology related to the rectum, including several colon ca. Besides doing the DRE you can get a good feel of where there wallet is, charge accordingly!! look forward to more emails."