By Howard Wolinsky
Can MRIs take over the heavy lifting in confirmatory biopsies? It depends on your Grade Group—it doesn’t do the trick for those with Gleason 2, favorable intermediate-risk cancers, but may be what the urologist ordered in Grade Group 1 (Gleason 6) patients.
Dr. Matthew Cooperberg, professor of urology at the University of California, San Francisco (UCSF), and colleaguesm reported in an abstract in the Journal of Clinical Oncology: : “Negative MRI—as defined by PI-RADS 1-2—does not consistently rule out the presence of GG≥2 prostate cancer and therefore cannot safely replace confirmatory biopsy. In some contexts (e.g., subsequent surveillance biopsy for patients with low [PSA Density], MRI may be an adequate surrogate.”
(The group also made a poster presentation at the American Society of Clinical Oncology (ASCO) Genitourinary Cancers Symposium in San Francisco in February.)
Cooperberg, urology chief at the San Francisco Veterans Affairs Medical Center, points out that Active Surveillance is “the preferred management” approach for patients with low-risk prostate cancer, and many with favorable intermediate-risk tumors.
“AS has been increasing in utilization both within the VA Healthcare System and nationally in the U.S. However, the limited data evaluating the quality of AS protocols suggests wide variability,” he noted. “One area of controversy is whether prostate MRI can replace prostate biopsy to guide decisions about whether to remain on AS.”
The researchers studied veterans diagnosed with Gleason grade group (GG) 1 or 2 prostate cancer at their diagnostic biopsy undergoing AS. The cohort was further limited to patients that underwent at least one post-diagnosis (confirmatory biopsy) and had at least one MRI with an assigned Prostate Imaging-Reporting and Data System (PI-RADS) score completed within 180 days prior to their confirmatory biopsy (CBx) and/or any subsequent surveillance biopsy (SBx).
They analyzed 1,439 MRI-guided confirmatory biopsies and 679 MRI-guided subsequent biopsies. The outcome of interest was grade group 2 or higher disease. The investigators considered PI-RADS 3 lesions or higher a positive test. The study covered 2013 through 2023, a period when prostate biopsies were becoming increasingly common.
The negative predictive value (NPV) was 74% for all confirmatory biopsies and 75% for subsequent surveillance biopsies.
“Performance was worse in some contexts: for example, among patients with GG2 at diagnosis, NPV was only 38% at the confirmatory biopsy and 60% at subsequent surveillance biopsies. On the other hand, for those with PSAD less than 0.15 ng/mL, NPV at the surveillance biopsy was 82%,” they said.
Cooperberg et al. concluded: “MRI was unable to consistently predict identification of [grade group 2 or higher] disease, and should be considered an adjunct to rather than replacement for biopsies on AS.”
Study limitations included the absence of data on Gleason pattern subtypes, biomarkers, or other pathologic findings such as perineural invasion.
The role of confirmatory biopsies in the time of MRIs remains an ongoing debate.
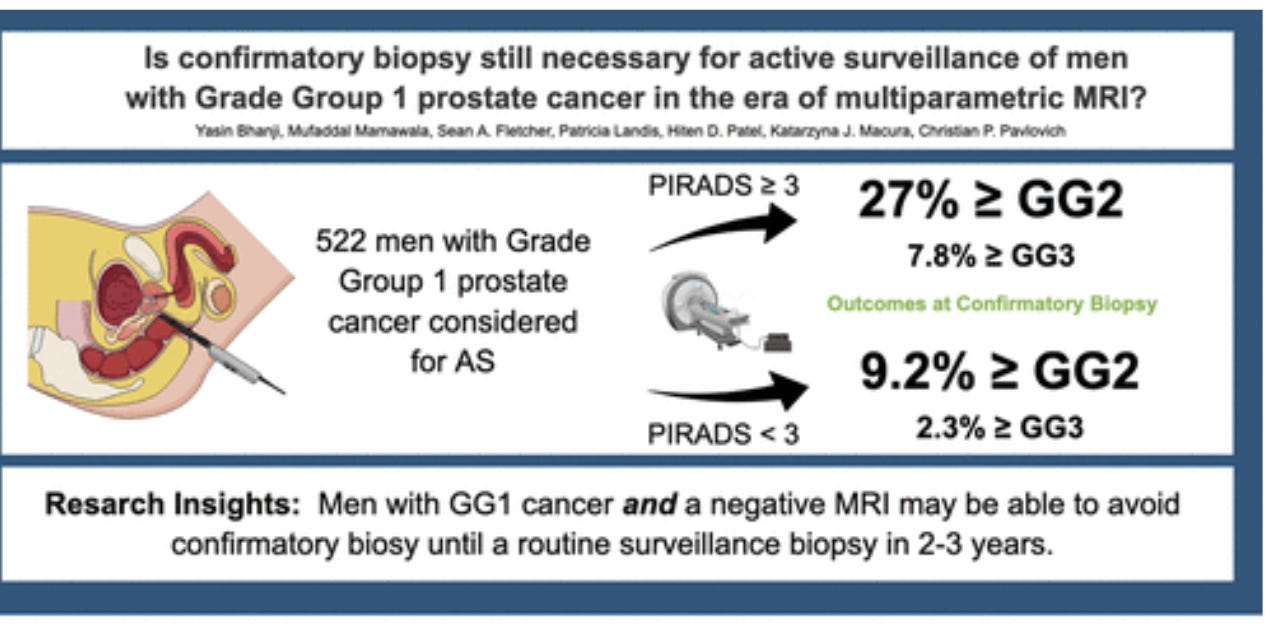
In a January 2025 study in the Journal of Urology, entitled, Is Confirmatory Biopsy Still Necessary for Active Surveillance of Men With Grade Group 1 Prostate Cancer in the Era of Multiparametric Magnetic Resonance Imaging?, Dr. Christian Pavlovich, head of the AS program at Johns Hopkins, the senior author, and colleagues, concluded: “Our data support systematic + targeted CBx for men with positive MRI considering AS, whereas men with GG1 cancer and negative MRI should be able to defer CBx.”
In fact, they said, “Our data support CBx (systematic + targeted) for men with positive MRI considering AS, whereas men with GG1 cancer and negative MRI may be able to avoid CBx until a routine surveillance biopsy in 2 to 3 years.”
So Grade Group matters.
The purpose of the study: “Men diagnosed with prostate cancer (PCa) considering active surveillance (AS) are recommended confirmatory biopsy (CBx). Whether this is necessary in the era of MRI-informed biopsies is questionable.”
Five hundred twenty-two men had GG1 PCa at diagnostic biopsies. At CBx, 20% reclassified to GG ≥ 2, 12% to unfavorable intermediate-risk (UIR) disease, and 5.6% to GG ≥ 3. Of the 306 with positive MRI (Prostate Imaging Reporting and Data System ≥3), 27% reclassified to GG ≥ 2 and 16% to UIR disease; men with negative MRI experienced these outcomes at rates of 9.2% and 5.5%, respectively.
There were no differences in reclassification outcomes based on MRI timing (and neither PSA density nor prostate volume added to MRI information. {Remember, Cooperberg et al. found: “In some contexts (e.g., subsequent surveillance biopsy for patients with low [PSA Density], MRI may be an adequate surrogate.”]
Still, Pavlovich told me the Cooperberg et al. seem “to echo what we found in our paper from Journal of Urology a few months ago. I can say that these preliminary data appear to support our paper that showed that GG1 patients with a negative MRI (PIRADS <4) can relatively safely delay a confirmatory biopsy (CBx) beyond 6-18 months, as they enter AS. However, similar GG1 men with a positive MRI should have that biopsy at 6-18 months after their first (diagnostic biopsy).
This gets into another controversy: Whether MRI-invisible lesions are even cancers.
“Also, while their abstract does not appear to go into the systematic biopsy outcomes vs targeted biopsy outcomes in men with a positive MRI, their group and ours I think prefer a systematic + targeted approach at DBx and CBx whenever possible.,” Pavlovich said.
He reports: “Reclassification rates at CBx were high for men with positive MRI but < 10% for any reclassification event in men with negative MRI. Our data support CBx (systematic + targeted) for men with positive MRI considering AS, whereas men with GG1 cancer and negative MRI may be able to avoid CBx until a routine surveillance biopsy in 2 to 3 years.
Mark Emberton, Dean, University College London Faculty of Medical Sciences, and professor of interventional oncology, Division of Surgery and Interventional Science at UCL, said the UCSF study “has a bit of an old-fashioned feel about it. They are doing two sets of random biopsies to find non-visible disease.”
Emberton, a pioneer with prostate MRIs and an advocate for ignoring invisible lesions on MRIs, added: “It is rare that we identify men with 3 plus 3 these days. They go away if you stop doing biopsies in men with normal imaging. If we don’t do random biopsies on the first round we are not going to do it on the second. My suspicion is that all non-visible diagnoses constitute overdiagnosis.”
More on invisible lesions here in Medscape.
More questions about confirmatory biopsies
By Howard Wolinsky
Confirmatory testing is standard after prostate cancer is diagnosed before Active Surveillance officially begins with surveillance biopsies.
But there are lingering issues:
—How long after diagnosis should confirmatory testing be done?
For example, the University of Pennsylvania tells its patients: “Sampling prostate tissue just two millimeters to the right or left of a tumor can affect the accuracy of your diagnosis — and whether active surveillance is best for you.
“That’s why we perform confirmatory biopsies. While they are not required by the National Comprehensive Cancer Network, the American Urological Association recommends you have one within two years. If we determine that Active Surveillance is best for you, you undergo a confirmatory biopsy within three to 12 months of your diagnosis.
“We use confirmatory biopsy to confirm the accuracy of the original biopsy. This approach ensures we don’t miss more advanced tumors. Confirmatory biopsies can also give you peace of mind that active surveillance is your best treatment choice.”
—Should the biopsy be transrectal vs. transperineal? The latest study by researchers from the University of Oxford reported that transperineal biopsies find significantly more prostate cancers than transrectal biopsies.
—Is biopsy the only way to confirm a cancer? Might magnetic resonance imaging (MRI) t be another option? A UCSF study found confirmatory MRIs don’t do the trick vs. confirmatory biopsies in men who have favorable intermediaterisk/Grade Group 2 and above while they might in those with Grade Group 1 cancers.. (See above.
Meanwhile, please answer my survey on confirmatory biopsies: https://forms.gle/E2AqLBK6hV21MVSV7
What else is news in low-risk PCa-land?
By Howard Wolinsky
—Throw me a lifeline. Please take the survey on your opinions on transperineal vs.transrectal biopsy: [https://forms.gle/T5pRqU5ravLVQ8xk7] This is a different survey from above.
This poll is being run in connection with a new British study that showed TP is better than TR in detecting prostate cancer:
Breaking: Transperineal biopsies find more prostate cancer, but also cause patients more pain and embarrassment
https://forms.gle/FjC4o6hWj2BZYhKN6
—Gotta’ have heart. Don’t miss the ASPI webinar on trying to fend off the greatest health threat we AS patients and most other prostate cancer patients face. It’s not prostate cancer. It’s heart disease. Dr. Darryl Leong, of McMaster U. (Go Marauders!), is a rare cardiologist who studies prostate cancer.
He is the featured speaker at Active Surveillance Patients International webinar from noon-1:30 p.m. Eastern on Saturday April 26. Register here: [https://zoom.us/meeting/register/xgT8w-i3Qp-iJkvOby0M9g]
—You’ve got guts. I have had my microbiome checked and reversed type-2 diabetes. How about you?
Researchers at University of California, San Diego are validating the gut microbiome—the community of germs in our gut that help keep us going— as a biomarker for prostate cancer aimed at men on Active Surveillance for low-risk prostate cancer. Participants get a free diet assessment/score, a microbiome report, and $25 gift card.
See if you’re eligible:
https://oncobiomix.studyenrollment.com
Is Auburn Tigers’ Coach Freeze in the ‘AS closet’?
By Howard Wolinsky
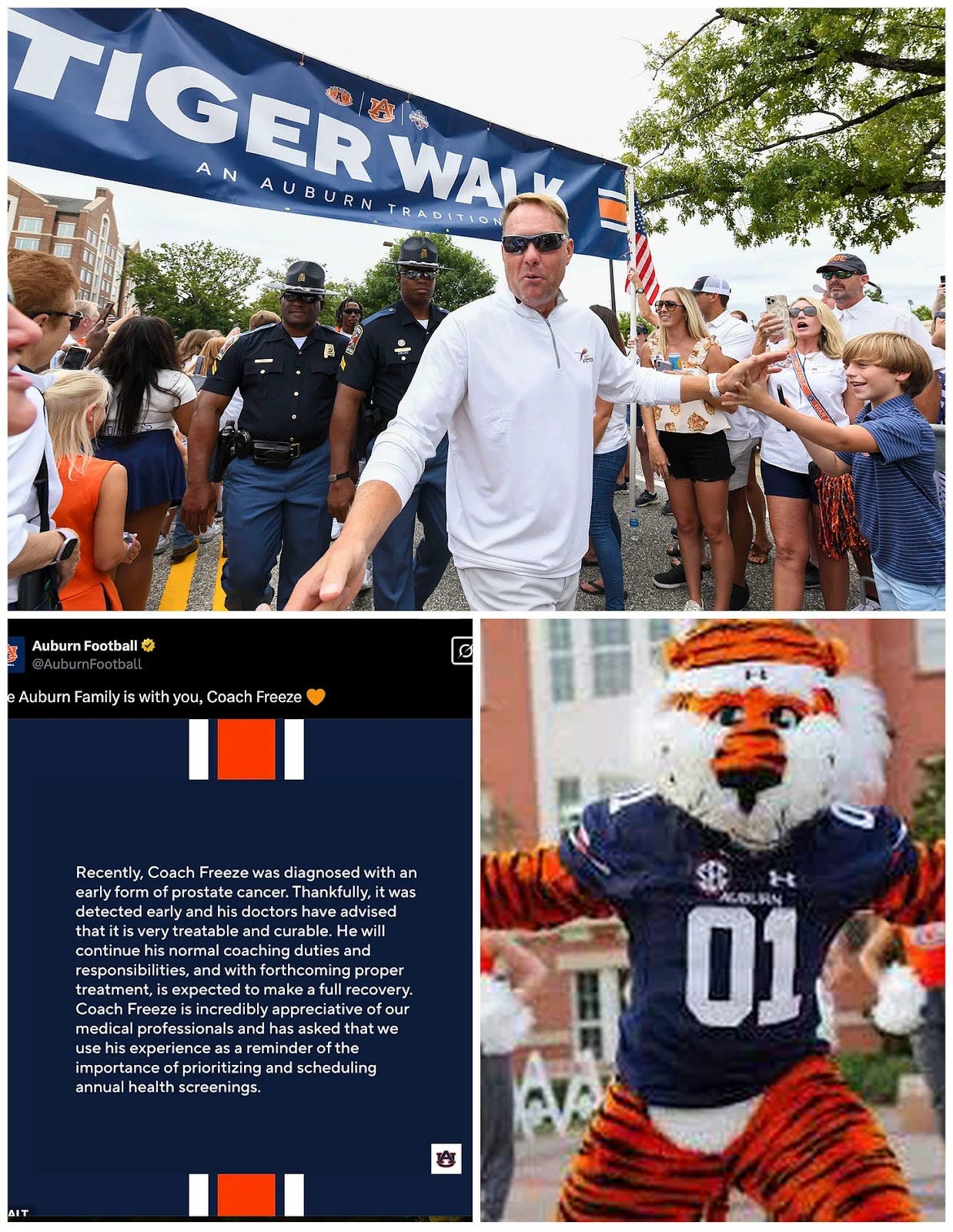
Back on February 28, Auburn University Tigers’ coach Hugh Freeze went public with his diagnosis with prostate cancer. It sounded a bit scary with talk about treatment and cures.
He and Auburn football’ss PR team sent a confusing message to anyone who knows about Gleason scores and PI-RADS: “Thankfully, [the cancer] was detected early and his doctors have advised that it is very treatable and curable. … He will continue his normal coaching duties and responsibilities, and with forthcoming proper treatment, is expected to make a full recovery.” {Emphasis added.]
Recovery? Cures? Treatment? Not aggressive?
What could the treatment be? Auburn and Freeze didn’t say.
And when I asked Shelly Poe, assistant athletic director-communications for the Tigers, said the Coach didn’t want to say more. She said: “He’s not interested in talking publicly about this until after he completes his course of treatment - thanks.” [Emphasis added.]
Of course that’s his choice.
Maybe Freeze became more comfortable and decided to talk to to a reporter from ESPN.
Sports reporters are more likely to write about Freeze’s losing seasons at Auburn and Freeze’s $45 million, seven-year contract than to ask in-depth questions about his prostate cancer, let alone know what questions to ask.
Freeze told ESPN his responsewhen he was diagnosed : "At the time, the only thing you hear is that 'C' word.”
Sound familiar? That’s how many of us react when we get the diagnosis.
ESPN’s Chris Low reported: “Admittedly rattled, and more scared for his family than anything else, Freeze has since settled on a course of treatment, and after getting some encouraging news recently from doctors that his form of cancer was low aggressive, he has decided to wait until January and let doctors reexamine his situation instead of having surgery.”
Freeze told ESPN: "I'm only 55. We're a family of faith, and I just didn't feel like it was time to rush into surgery. I'm at peace with it."
Freeze apparently has a sleepy lion brand of prostate cancer rather than the snarling tiger.
He wisely has deferred treatment to monitor his cancer,
Sounds to me as though he is in the “AS closet.” Many men, maybe especially those in the public eye don't go full monty with a low-risk diagnosis and management with Active Surveillance.
Why? They want to preserve their privacy--at least to a point. They want to avoid job discrimination and other financial toxicities and steer past the stigma of prostate cancer.
Brian Helfand, MD, PhD, head of urology at Endeavor Health in the Chicago area and an AS expert, read the ESPN article and told me: “I think he is on AS. It’s not entirely clear from article, but it hints at it.”
The reporter may not have known the fine points, nor realized he had a bit more of a scoop than he realized.
(Clockwise: Coach Hugh Freeze, Augbie the snarling tiger mascot, X post on Freeze.)
I contacted Poe again and asked if the Coach would be willing to talk and maybe confirm he’s on AS. She told me: “He’s not interested in getting detailed at this time - thanks.”
Does this mean “nevermore,” as the raven said in that famous poem by that other Poe. I hope not.
Maybe Freeze eventually will start winning championships, open his kimono, emerge from the AS closet, and tell the public his full story with PCa.
It could be a boost for AS and spare more men from the potential side effects from surgery and radiation.





It is tough for patients to decide when the research is conflicting and protocol and doctors vary.
Thank god for Emberton! At my most recent AS check up my Uro suggested a biopsy. She was talking about a BLIND TRUS!!! Just ridiculous. Not going to happen. In fact, I am beginning to get leery about MRIs, mainly over the Gd contrast. The Microultrasonography guided biopsy needs to get more attention and funding.