Dan Dressen's six-year active surveillance journey--and still counting
Cancer was there. Then, poof. It was gone. Could diet have done the trick?
(As a medical journalist, I always try to include patient anecdotes in my articles. They make the stories more real. Now I am a graduate student in the Master’s in Public Health Program at the University of Illinois@ Chicago. I learned that story-telling is an important part of understanding and developing programs to serve the public health. Researchers call it “qualitative research” as opposed of course to “quantative research” that’s all about the numbers.
(Without qualitative research, important studies like the ProtecT trial, proving the safety of surveillance, could never have worked. My friend Dan Dressen here shares his surveillance journey, which should help others along the path of surveillance. Dan has an amazing story—about how his Gleason 6 lesions were there—and then they weren’t. He’s a steady and well-informed hand as a moderator for AnCan Foundation’s Active Surveillance Virtual Support Group. We meet at 8 p.m. the first four Wednesdays of the month in the Barniskis Room.
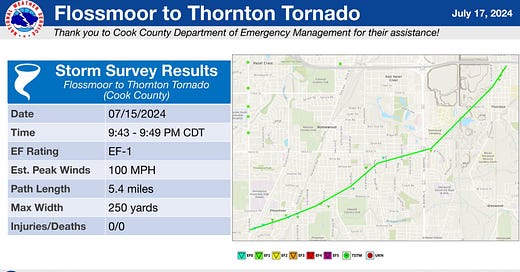
(NOTE: Meanwhile, I’ve been through a bit of an ordeal. While I was recuperating from COVID-19—my first bout—a pack of 20+ tornados roared through the Chicago area, including an EF1 with 100 mph winds that hit my southern suburb, Flossmoor. We lucked out. Our house was intact though many trees were uprooted. We were without power for four days so I couldn’t post the newsletter. Our sons persuaded us we were in danger from the heat and needed to leave. I listened to them and I’m grateful. My quarantine ended so we escaped to Michigan, the Land of Bountiful Bandwidth and Icy AC. Hope things will return to normal this week. And I wish all of you all health—and safety. Howard Wolinsky)
Take it away, Dan:
By Dan Dressen
In the fall of 2017, I turned 65 and thus became eligible for Social Security. This required me to see a doctor to get a check-up. During my 11/16/2017 doctor visit, a couple of blood samples were taken, including a sample to be used to check my PSA (prostate-specific antigen). At 6.65, my PSA was a bit high so my doctor put me on an antibiotic for 2 weeks. The thought was that the raised PSA may have been caused by an infection and for that reason the antibiotic. On 12/4/2017, I had my PSA checked again, and this time it was 4.02, still a little high and I was referred to a urologist. Three days later I saw a urologist and was scheduled for a prostate biopsy.
(Lila and Dan Dressen in Music City, Nashville.)
Five weeks later, on January 4, 2018, I had a transrectal (TR) prostate biopsy. The antibiotic known as Ciprofloxacin, or Cipro, was prescribed which was to be taken both before and after the biopsy to mitigate the chance of an infection. A week later, on January 11, I saw my urologist to go over the results of the biopsy. He had taken 12 cores and of those 12 cores, two cores were determined to have cancer and the amount of cancer in those two cores was 20% and 2%. Whatever we discussed was new to me. It was determined that I was a candidate for Active Surveillance (AS). Being on AS meant that going forward I would be having my PSA checked every six months and would be getting periodic MRIs. My Urologist also prescribed finasteride, to be taken for an enlarged prostate which was determined to be 66 grams in size, 20 to 25 is normal. The doctor also told me he was taking finasteride for his thinning hair. When he told me that, I was on board with the drug. (I would later learn that finasteride is a hormone and the dosage for hair is 1 mg./ day and 5 mg./ day is for an enlarged prostate.)
A few weeks after my prostate cancer (PC) diagnosis, my wife Lila, noticed a PSA (Public Service Announcement - the other PSA) in the local newspaper, for a Prostate Cancer Support Group meeting in the town of Davis, where we lived. I attended that meeting and from there I learned of another monthly PCSG meeting in Sacramento, 3 days later. I also attended the meeting in Sacramento. At these meetings, I heard the personal stories of men who had PC like myself. Most of the men had more advanced PC so I didn't feel their stories applied to me, yet it was eye-opening as to how serious PC can be. There was one guy who was at both the Davis meeting and the Sacramento meeting. I commented to him that he was at both meetings. He replied that he was also a regular at two other monthly meetings in the Sacramento area, for a total of 4 different support groups. I would later learn how high Charles's PSA had gotten. When PSA goes above 10 -15, it becomes a concern. Charles's PSA had gone above 5,000. (More about Charles later) Hearing the stories from the men with more advanced PC made me a bit uneasy about my disease even thou I qualified to be on Active Surveillance.
At that very first meeting in Sacramento, a video was shown that very much affected me and how I dealt with my cancer. The video was of Dr. Charles "Snuffy" Myers telling his story of how he had advanced PC and how he defeated it. What I mostly remember from the video was the changes Dr. Myers made to his diet. He talked about foods that were beneficial and foods that were bad for men who had PC. He said foods that were high in Omega 6 were bad. He said, "Omega 6 adds fuel to the fire". I very much took that to heart. Corn is high in Omega 6, so for me, it's no more sweet corn in the summer, no more cereals based on corn and no more popcorn, my favorite snack food. At some point in 2018, my urologist would also advocate for a more vegetarian diet and Walnut Milk as a substitute for dairy milk. But by then, I already had discovered flax milk which has 120 % more Omega 3, the good Omega, than walnut milk. (500 mgs vs 1,200 mgs) A year later in 2019, I would also go to a more vegetarian diet, also omitting most dairy products.
In January 2019, I had my first prostate MRI. It was one year after my biopsy and it was assigned a grade of PI-RAD 2 on a scale of 1-5. PI-RAD is short for Prostate Imaging - Reporting and Data System. Pi-RAD 2- low implies clinically significant cancer is unlikely to be present.
Also in the middle of 2019, I chose to go on a mostly vegetarian diet. By this time I've had my PSA taken 5 times. (6.65, 4.02, 2.61 2.06, 3.17) The average score of the 2 Pre-finasteride PSAs was 5.33. The 3 PSAs, after taking finasteride averaged 2.61. As expected, the finasteride reduced my PSA by approximately half.
In December of 2019, I was to have a minor arthroscopic surgery on my knee. This procedure required that I have an EKG before the surgery. It was in the course of having an EKG that I noticed an increase in breast tissue. Not sure how, but I became aware that the finasteride I was prescribed, is a hormone that can cause a multitude of side effects known as "post-finasteride syndrome". An increase in breast tissue, known as Gynecomastia, is one of the potential side effects. The likelihood of this potential side effect is quite small. I've seen it stated as "less than 1%", "1/2 to 1%" and "less than 10 in 1,000".
2020 was a strange year. It marked the beginning of the COVID shutdown. The in-person support group meetings would be suspended. My wife and I started the process of moving to a new state and new doctors. From the middle of 2019 and through 2022, I would continue checking my PSA and have another prostate MRI. The 2nd MRI in 2021 was again graded PI-RAD 2. During these 2&1/2 years, my PSA was checked 5 times (2.14, 1.59, 1.67, 1.18, & 1.42) with the average PSA score being 1.57. During that time, and being on a vegetarian diet, my average PSA score decreased by approximately 35%.
In 2022, I was a little concerned about the possible side effects of the finasteride that I was taking. With the approval of my new doctor, I decided to reduce the dosage from 35 mg. /week to 10mg. /week, a reduction of 70%. Between 4/2022 and 7/2023 I had my PSA checked 4 times (1.41, 2.01, 2.04, & 2.46) and as I expected, my PSA did rise, but I was comfortable with the amount it rose.
When first diagnosed in 2018, I started going to two different "in-person" PC support groups. Since 2019, I have been listening to "Men's Health", a weekly program on the Sirius XM Doctor Channel. My favorite radio host is Dr. Stacy Loeb. Her specialties are prostate cancer and research and prostate cancer is often the subject of discussion when she is the host. Four years ago in 2020, I discovered the AnCan (Answer Cancer). AnCan has multiple online support groups, including a group specific for men on Active Surveillance.
It's 2023, and after taking in much information related to PC and my situation, I realized that I never had a "confirmatory biopsy,” which should have been done within about a year of my first biopsy in 2018. I also heard uropathologist Dr. Jonathan Epstein, say that biopsies should be done every 3 or 4 years and it's been 5 1/2 years since my only biopsy. I present this to my new urologist, Dr. Joel Hancock, who is young and has a private practice. Dr. Hancock does not see an urgency for a biopsy considering that my PSA has stayed low. But, he goes along with me getting an MRI. Getting an MRI before a prostate biopsy is the correct approach regardless and so my doctor orders an MRI. The prostate MRI comes back PI-RAD 4 which indicates a 60% chance of significant cancer. Now Dr. Hancock is on board with me getting another biopsy. From my support group meetings, I learned that a transperineal biopsy was preferred to a transrectal biopsy because of less risk of sepsis and other infections. When I first started seeing my new urologist in 2021, he did not do transperineal biopsies. But now, in 2023, he does TP biopsies. I wanted to have what is known as an MRI-guided TP Biopsy. Dr. Hancock does what is called Cognitive Fusion TP Biopsy. The Cognitive Fusion relies a bit more on the skills of the doctor doing it. I trust the knowledge and skills of my new doctor so I'm OK with him doing a Cognitive Fusion TP biopsy. Besides, I won't have to travel two or three hours to Boise or Salt Lake City for an MRI-guided TP biopsy from a doctor that I do not know. So a TP biopsy is scheduled to be done in October.
On October 3, 2023, I had a transperineal prostate biopsy in my urologist's clinic. 20 cores are taken. 16 cores are taken systematically and 4 more are taken, 2 each in the 2 areas of concern. On October 12, I see my urologist to review the biopsy results. The result is "no cancer found" in the 20 cores taken. I did not expect that! That same day, I had the prostate cores sent out for a second opinion from Dr. Ming Zhou at Tufts University. (Zhou is now at Mt. SInai in New York.) Two weeks later Dr. Zhou reported back and confirmed the biopsy results of no cancer detected.
There was a study of 1,595 men done between June of 2012 and June of 2016. "Results: Of 497 men, 88 (18%) with PI-RADS 4/5 abnormality, prior to initial biopsy, had no cancer on magnetic resonance imaging targeted prostate biopsy." A follow-up study was done with a small number of men with "no cancer detected". In that follow-up study, both low-grade and high-grade cancer was found and still, some men had no cancer detected. My takeaway from this study is that even though my last biopsy did not detect cancer, I will continue with being on Active Surveillance.
I earlier told you about Charles who had a PSA of over 5,000. He was a guy I came to respect and will always remember. Charles was a regular at four different PC support groups in the Sacramento area and seemed to know as much about his disease as the doctors. A few months after I started going to PC support groups another guy started attending, his name was Gregg. Gregg had been diagnosed with PC shortly before he started coming to the meetings. He had a PSA that was over 800 and he was sort of a wreck, emotionally. Easy to understand why he was upset. As I saw it, Charles sort of took Gregg under his wing, so to speak. I would soon see them coming together to the two different support group meetings that I attended. I would see Gregg eventually accepting the cards he was dealt. But then, at the very last "in person" support group meeting, that I attended, in early 2020, Charles announced that his skin cancer returned and he was "afraid.” This was just before COVID shut down "in-person" support groups. Because of COVID and relocating to a different state I sort of lost contact with the PC support groups. In 2022, I learned that Charles had lost his fight with cancer in January of 2022. But then something happened. I would attend a few of the "online" PC support groups. I then found Gregg had taken on the role that Charles once had. Gregg was now calm about his disease. He said he was taking it "day by day". But still, sad to say, Gregg would eventually lose his fight with cancer in April of 2023.
To end, I would like to thank and acknowledge some people who helped me along the way:
Beverly Nicholson: Beverly is a registered nurse who has led the Sacramento PC Support Group for more than 30 years.
Rick Davis: Rick is one of the founders of AnCan (Answer Cancer). AnCan has more than a dozen different support groups, including three that are specific to three different levels of Prostate Cancer.
Howard Wolinsky: Howard is a medical writer and fellow patent. He writes about the ever-changing advances in dealing with prostate cancer and brings his experience to the AnCan PC Virtual Support Group for AS, which he co-founded.
AnCan Active Surveillance Support Group Moderators: These guys give of their time to share personal stories and experiences with others who attend the online meetings, giving extra attention to those who are newly diagnosed.
Dr. Joel Hancock: Due to prostate cancer and kidney stones, I've seen Dr. Hancock more than a dozen times in the last 2 1/2 years. I'm very glad to have him as my urologist, a doctor I both like and trust.
Dan Dressen grew up St. Bonifacius, Minnesota (population 600). When he was 24, he put his tools, guitar and clothes in a ‘73 Toyota Corolla and left for California. The journey took a couple of months as hetook a detour to Maine, passing through Chicago, DC & NYC along the way. He turned 25 while passing through Craters of The Moon National Park in Idaho. He eventually ended up living and working in both Southern and Northern California. He met Lila,his wife of 34 years, in SoCal. They now live in a small town in Idaho, a two-hour drive from that park where he turned 25 some 47 years ago.
Watch Solo Arts Heal featuring a performance by Dan Dreseen: https://ancan.org/solo-arts-heal-with-dan-dressen/?mc_cid=62fa155a13&mc_eid=50a6c1c606
Please answer a brief survey on AI and urology
Peter Evancho, an attorney and second-year medical student at the University of Maryland, Baltimore, is conducting a policy analysis about AI and urology and is asking for our help.
Can you take a few minutes and answer Evancho’s survey and share your thoughts about AI and urology care?
Here’s what Evancho has to say about himself and his survey:
“My name is Peter Evancho, and I am a second-year medical student at the University of Maryland School of Medicine. In conjunction with the Department of Surgery and the Division of Urology at the University of Maryland Medical Center and Principal Investigator Minhaj Siddiqui, MD, I am conducting a short survey to examine the the integration of artificial intelligence (AI) into urologic practice and understand both its promising advancements and the substantial ethical, legal, and regulatory challenges it poses. Your insights are crucial, and the survey is designed to be completely anonymous. Participation is voluntary.”
Survey Link: https://rs.igs.umaryland.edu/surveys/?s=3R37KJMPERYEWMH9
The survey will remain open until September 1, 2024. The University of Maryland, Baltimore’s Institutional Review Board has approved this study under HP-00109759
Webinar on 2nd opinions. My opinion? I’m going, why not join us?
By Howard Wolinsky
Active Surveillance Patients International (ASPI) is holding a patient webinar at noon EST on Saturday, July 27, called “In our opinion, get a second opinion.” Register here: https://zoom.us/meeting/register/tJUkdOqpqT0iGNHcOP4sfLoiIsdIp-nLwbUS
Four patients will share their experiences with prostate cancer and how second opinions—or their absence—had a huge impact on a patient’s fate.
I will be on the panel along with my Chicago area friends, retired attorney Jim Schraidt, a former ASPI board member and current ZERO board member, who like me was diagnosed in 2010 but went on a different path that transformed him into patient advocate supreme for Active Surveillance, and newly diagnosed PCa patients Charles Brown III and Keith Day, whose second opinions saved them from the robo knife and the ray gun.
Micro-ultrasound webinar
By Howard Wolinsky
Micro-ultrasound is an amazing tech that is catching on slowly and may be giving MRI a run for the diagnostic market.
Dr. Ravi Kumar, a urological oncologist on staff at Humber River Hospital in Toronto, is making a presentation on the status of micro-ultrasound, “ExactVu Micro-Ultrasound: A new frontier in urological imaging” at 7-9 PM EST Wednesday, July 24. Register here: https://conta.cc/4co75TY Prostate Cancer Support Toronto is sponsoring the meeting.
(Dr. Ravi Kumar)
Humber River Hospital is North America’s first fully digital hospital, using the latest tech to enhance all aspects of quality patient care delivery, improving efficiency, accuracy, reliability and safety.
ZERO needs your help in Congress funding CDC on PCa issues
By Howard Wolinsky
The House Appropriations Committee has made significant cuts for Fiscal Year 2025 to the Centers for Disease Control and Prevention (CDC), nearly a quarter of its funding.
Among other things, the CDC supports a number of prostate cancer activities, including outreach into high-risk communities and support for state and local prostate cancer programs, all of which are at-risk for large cuts.
I have some skin in this game. I helped win a $1 million grant from CDC—the first of its kind—to study opinions about Gleason 6 (Grade Group 1) in African American and Hispanic men.
Zero said: “Your elected officials need to hear from you - these programs are critical for improving prostate cancer outcomes and saving lives.
”The Senate is next to weigh in on funding for CDC. We can help protect prostate cancer funding by telling Senators that cuts would be devastating for our community.”
Please check in here: https://p2a.co/15HnJhg







Dan,
Thank you for sharing your story with us, glad to hear your diagnosis of "no cancer found", what a relief that must have been!
Howard,
Thanks for allowing patients to share their stories! It's nice to know what other guys are going through.
Howard,
I appreciate you writing my story about being on Active Surveillance for 6+ years. It's been an interesting experience, and I've been sending it to others who might have interest.
Thanks, Dan