By Howard Wolinsky
I want to let you in on a dirty little secret about active surveillance (AS).
First, the bad news: The dropout rate in the past has been high, according to a just-released study. Really high.
Now some better news: The dropout rate likely has been dropping as AS has caught on in recent years in the U.S. and better imaging is available. We’ll have to keep monitoring these numbers.
I spoke recently to urologist Rashid Sayyid, MD, MSc, a fellow at Princess Margaret Cancer Centre in Canada, who reported on a study with the latest (but somewhat dated) figures on the dropout rate from AS. He presented his research at the American Urological Association meeting in May in New Orleans.
He and his co-authors, including AS “father” Laurence Klotz, MD, of the University of Toronto, looked at what happened in the long run to low-risk patients with Gleason 6 scores and PSAs less than 10 in the Surveillance, Epidemiology, and End Results (SEER) Prostate with Watchful Waiting database between 2010 and 2015. The patients had been managed with AS for at least one year following diagnosis.
Sayyid told me that almost two-thirds—a whopping 64%—of these patients left active surveillance within ten years of diagnosis.
Most leave AS because their cancers have “progressed” or their PSAs have been rising.
Some may leave AS because they are anxious, depressed, or distressed. Their cancer is making their lives miserable. They simply can no longer co-exist with their cancer. So the cancer has to go.
Could some, or many, of these patients have stayed on AS if they got help coping with their mental discomfort? Check out his article on anxious surveillance:
What are your expectations with AS?
I had great expectations. My doctors told me that I have very low-risk Gleason 6, meaning a single positive core with less than a millimeter of Gleason 6 “cancer.” (Note: Some urologists don’t consider Gleason 6 lesions to be cancer at all.)
My so-called cancer has not been seen with a biopsy or MRI since it was first confirmed in 2010—though my urologists assure me the slow-growing cancer is still lurking in there.
Since I first went on AS, my urologists have told me I likely will be able to live with my Gleason 6 and will die from something else, most likely heart disease.
We don’t get out of here alive. But we have to realize that we toss the dice in the craps game of prostate cancer, and we each react our own way.
It’s a bit like a telenovela, those popular Latin American soap operas, filled with twists and turns. “The Days of our (Prostate Cancer) Lives.”
AS mileages vary. AS has been not only for very low-risk patients with a little Gleason 6 but also for those with high-volume Gleason 6 as well as those with favorable Gleason 3+4 intermediate-risk prostate cancer. (If you don’t know where you’re at, ask your doctor for your score.)
I had imagined those of us with low-risk prostate cancer would be surveilling into the sunset, or at least until we transitioned into less aggressive management of our lesions, such as watchful waiting sans the regular digital rectal exams, PSAs, MRIs, and biopsies.
Enter stage left: Dr. Kirsten Greene
Kirsten Greene, MD, chair of urology at the University of Virginia, provided some warning about this in a webinar I moderated for AnCan in our New Year’s Eve session in 2021. She explained that in her view the overarching goal in AS is to delay the use of treatments, meaning radiation and surgery, without compromising patients' long-term survival.
In the view of some, maybe many, doctors, the goal isn’t necessarily to stay on AS for the rest of our lives.
It was a shocker for many of us. Say it ain’t so, Dr. Greene. I wrote her a follow-up note and asked her to repeat, explain and confirm what she said.
(Kirsten Greene, MD)
Here’s what she told me: “Regarding the issue of deferring treatment vs. avoiding treatment, this goes to the heart of active surveillance vs watchful waiting (WW). For people who believe they are avoiding treatment forever, perhaps they are on watchful waiting. It is at least worth a conversation with their urologist to see which one they are really on and why.
“Sometimes we (physicians) are not great about communicating why we think someone ‘will never need treatment in your lifetime.’ Maybe it isn't so much about the prostate cancer risk as it is about patient age and competing comorbidities.
“Patients may think that the cancer just isn't that dangerous while the physician is thinking about competing health risks vs. the cancer. This is why I stressed so strongly that patients should know if they are on AS or WW and to be sure it is the one they want. I am basing this statement on all of the long-term active surveillance trials and cohorts which have been published as well as my participation in one of them (UCSF) and my experience as a urologic oncologist.”
Greene cited research from the Johns Hopkins active surveillance cohort, one of the most conservative, meaning that low-risk and very low-risk patients were included but very few with intermediate-risk patients. The study ran from ancient AS times (1995) through 2018, as AS was finally starting to gain momentum in the U.S.
Greene noted that in this group, 35% had gone under the knife or the radiation beam at five years, 48% by ten years, and 52% by 15 years. “The converse is the answer to the question of what percentage of men avoid treatment for each time point,” she said.
That’s one snapshot of the dropout rate at one institution, an early advocate for AS.
Sayyid presents a different snapshot, one derived from a national database disclosing an even higher dropout rate of up to two-thirds at 10 years vs. about 50% at Hopkins at the same point.
Running the race with AS
AS may be more of a sprint than a marathon for many AS runners.
Many of us anticipate living with low-risk prostate and never being treated. In other words, we thought we could live with Gleason 6 lesions for the rest of our lives as we get picked off by other causes.
These studies are a reality check. Some patients who opt for treatment as soon as they were diagnosed have experienced decisional regret and wished they had delayed treatment and had extra months and years on AS before being treated.
Some, maybe many, doctors see AS as a temporary port in a coming storm, and that patients on AS may be treated, possibly sooner rather than later than we thought. (Please use the comment bubble to describe your expectations.)
Consider all the effort that had gone into persuading men to go on AS with the goal of sparing them—at least for a while—from the risks of surgery and radiation, including such buzz killers as erectile dysfunction, incontinence, and rectal issues.
Sayyid and colleagues said: “Patient factors influencing decision to opt for definitive therapy, and, specifically, choice of radical prostatectomy (RP) versus radiation therapy (XRT) remain unclear.”
Not all AS patients are created equal
Kevin Ginsburg, MD, a urological oncologist at Wayne State University in Detroit and one of the drivers of the successful MUSIC (Michigan Urological Surgery Improvement Collaborative) program in which a whopping 91% of eligible candidates in Michigan go on AS, gave me another take on whether he expects patients with low-risk Gleason 6 are on AS for good or just temporarily
(Kevin Ginsburg, MD)
He said, “A little of column A and a little of column B. I often explain that the goal of AS is to avoid or delay treatment, potentially forever, or until the point where a clinically significant disease is found that should then be treated. For some men, that delay is indefinitely, and they can/should remain on AS for the remainder of their lives. For other men, if clinically significant disease is found in the future, it may be very appropriate to seek treatment and leave AS.
“Some men may leave AS because of grade progression and treatment at that point. All the data would suggest that these men are no worse off for delaying their treatment until if/when it’s needed. But they have had serious gains in quality of life while they have been on AS. I look at that as the success of AS and not a failure.“
Sayyid told me: “Not all active surveillance patients are created the same. I think about it from two different perspectives – one from a disease process. You told me you were initially diagnosed with low-volume [single core, less than 1 mm) Gleason 6.
(Rashid Sayyid, MD)
“That is not the same as being diagnosed with, let’s say, two cores of Gleason 7, where we’re talking about, hey, can we buy a couple more years potentially of maintaining erectile function, avoiding urinary incontinence?
“Hopefully, we never have to, but odds are that we may have to treat you if you show volume or grade progression or something more worrisome on your imaging. Whereas, having that conversation with somebody who has low volume Gleason 6, we need to consider those two patients as two different entities.”
Progession
Progression? What is progression? Maybe it’s not what you think.
First, here’s what it usually isn’t: Conversion of lazy Gleason 6 lesions into menacing metastatic killers. Doctors like Klotz and my own urologists assure us that it is virtually unheard of for a Gleason 6 itself to spread and become a threat to our lives. They say Gleason 6 lesions don’t have the “machinery” to do that damage.
Now, here’s what progression is: the discovery in a patient on AS of more advanced cancers that can spread and kill.
Data not perfect
Sayyid also noted there are some problems with the SEER database he used: It’s not fully representative of the U.S. And the results are not necessarily representative of what happens in academic centers. He said urology practices outside the academic centers may lag by a decade behind what is happening in centers of excellence.
His study used the most current data available before AS became the choice of the majority of low-risk patients (60%, per the American Urological Association’s AQUA database in 2021).
Sayyid started his study in 2010--when maybe 6% of candidates for AS actually chose the then-unbeaten path--and ran into to 2015 when 32% opted for AS.
In the next six years, AS soared in the U.S. to 60% of men with low-risk Gleason 6. It’s hoped to reach 80-90% of the U.S. low-risk “market” in the near future.
AS dropout rate lower now?
Sayyid also said he suspects the dropout rate is lower now as cancer detection has improved with wider adoption of AS itself, and adoption of MRIs and targeted biopsies. But we don’t know that for sure yet.
“It’s going to be lower now. It goes back to a point that I was mentioning when we talk about volume or grade progression for a patient on active surveillance; I think it’s first and foremost historically been an issue of poor detection, underdetection. MRI is a whole game-changer right now in this disease space.”
AS dropout rates, like AS uptake rates, vary by country and even by individual doctor’s practice. While the U.S. has an AS rate of 60% now in patients with low-risk cancer, the VA system has 70%. The state of Michigan, through the efforts of the MUSIC program, is at 91%, comparable to national rates in Sweden, the United Kingdom, and Holland.
Some individual urologists report uptakes of AS reaching nearly 100%. But their patients may select them because they are known AS friendlies.
Filling the GAP
Movember Foundation's Global Action Plan Prostate Cancer Active Surveillance GAP3 consortium looked at the issue in 10,296 men on AS from 21 centers across 12 countries. These numbers include data from the U.S., Canada, Australasia, UK, and Europe from 2014-2016.
These researchers reported in 2019: “Our descriptive analyses of current AS practices worldwide showed that 43.6% of men drop out of AS during 5-yr follow-up, mainly due to signs of disease progression.”
(There’s the “P word” again.)
Their breakdown was:
-- 28% of the men showed signs of disease progression
--13% converted to active treatment without evidence of progression
--2% continued to watchful waiting, and
--2% died from other causes.
The remainder were on AS at the five-year point.
The cumulative incidence of progression was 28% at five years, and 38% at ten years.
More snapshots
Here’s more on dropout rates, which seem to be also all over the map depending on your doctor’s philosophy on AS and practice trends based on where you live.
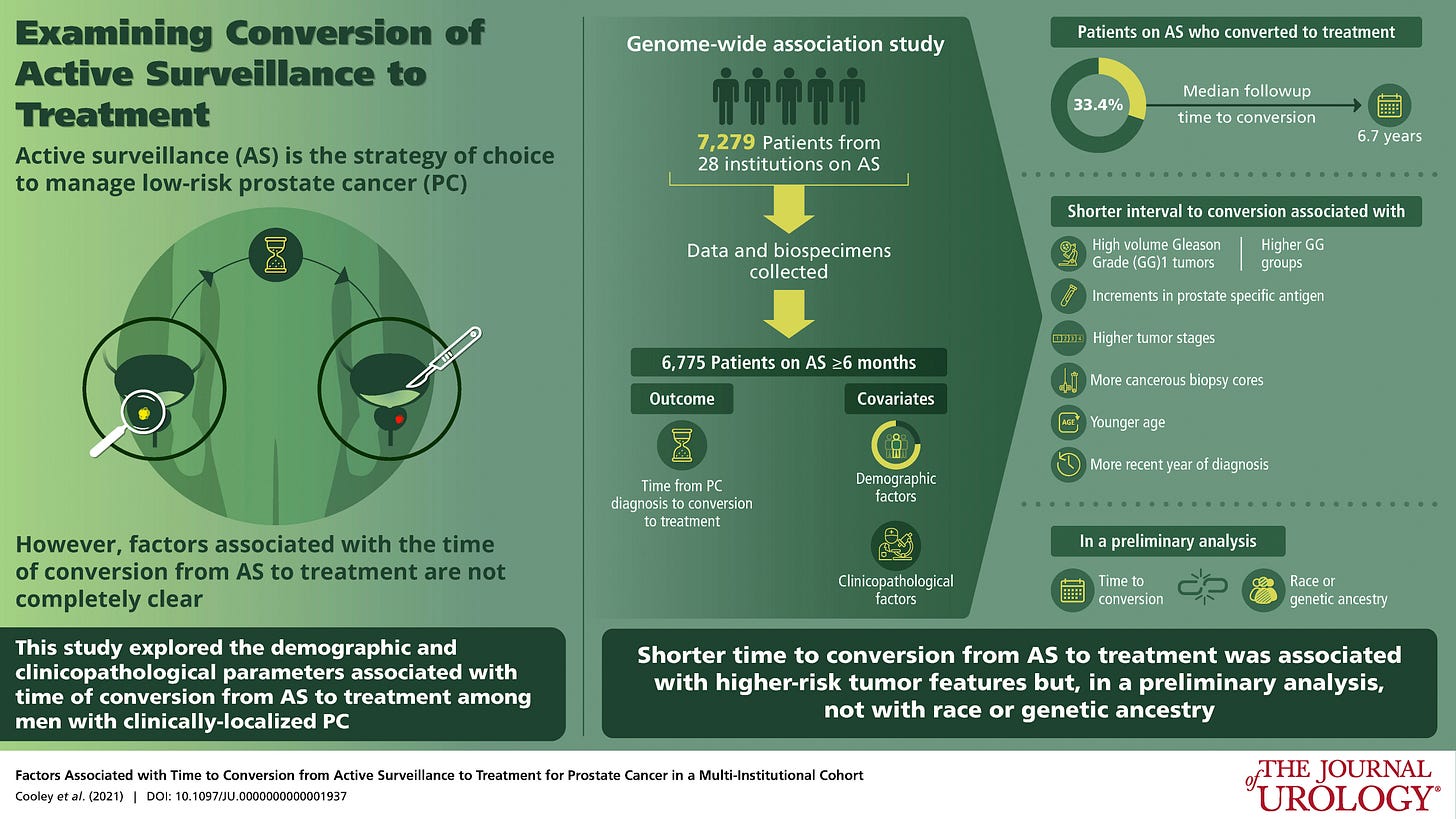
A major multi-center study of five-year follow-ups led by Lauren Folgosa Cooley, MD, of the Department of Urology, Northwestern University Feinberg School of Medicine in Chicago, under famed urologist William Catalona, appeared in the Journal of Urology last year.
Cooley reported that the most common reason for “conversion”--seeking definitive treatment-- was grade reclassification alone (48.8%), followed by PSA progression (8.5%), tumor volume progression (7.2%), anxiety (5.0%), and other reasons (9.0%).
(Note the mention of anxiety as a cause. Not all researchers mention anxiety.)
This was early in the AS boom. Researchers looked at stats from 2014-18.
Conversion. Sounds like a religious experience. Like my ancestors in Spain at the time of the Inquisition—you’ve heard of the Spanish Inquisition? as Monty Python asked—I don’t want to convert to prostate treatment. I won’t unless I have a spike in my PSA and an MRI and biopsy confirm I have trouble brewing.
A Canadian study at the Princess Margaret Cancer Centre Quality of Care Initiative on Active Surveillance, published last year, showed after a median follow-up of 48 months, 4,337 (51%) patients had discontinued AS.
Researchers added: “Factors associated with AS discontinuation were younger age at diagnosis, year of diagnosis, higher comorbidities, treatment at an academic center, treatment by physician and institution in the highest volume tertile, and adverse cancer-specific characteristics (higher prostate-specific antigen [PSA], a higher number of positive cores and a higher percentage of core involvement at diagnosis.”
This study, which does not mention anxiety, ran from January 2008 through December 2016, in Canada, where AS uptake is much higher than in the U.S. (70-80%).
Drop out?
Sayyid had some good news: With AS growing and the implementation of MRI on the rise, and let’s add the growing popularity of genomic and genetic testing in the U.S., doctors are getting better at finding those of us who are good candidates for AS and those who should consider treatment.
A few years ago, my wife Judi and went on a trip to Costa Rica. We stayed at a resort where the water and pools were heated by the nearby (active) volcano.
On the grounds, there were clear glass cases containing helmets. In case of a major eruption, the idea was to break the glass and don the helmet.
I concluded that this was kind of a joke. Debris, such as rocks and lava, spewing from the volcano would come at you at the speed of light. You wouldn’t have a prayer to put on a helmet.
I took solace in a sign posted in the rooms that said “Mantenga la calma.” Remain calm.
I wouldn’t freak out over the dropout numbers. Ride the AS wave as long as you can or want. Take more aggressive measures if needed. Mantenga la calma.
How Active Surveillance programs can reach 90%-plus of low-risk patients
Yet U.S. uptake for AS is only 60%
By Howard Wolinsky
The Active Surveillance Coalition, a collaboration of leading support groups for active surveillance (AS) for prostate cancer, is sponsoring a webinar at 9 a.m. Vancouver/12 p.m. New York/5 p.m. London/6 p.m. Amsterdam on Thursday, Nov. 17 to discuss how we can move the needle on AS, close monitoring of prostate cancer.
AS leaders from Sweden, Holland, the United Kingdom, and the state of Michigan’s MUSIC program will share their “secret sauce” for reaching AS rates of near 90% and above.
The free webinar is entitled “Moving AS to the next level: Can we help more patients?”
Register here:
The United States has lagged behind wealthy countries in AS though the approach started there and in Canada in the late 1990s. AS uptake with AS finally reached a majority of 60% in 2021 with the American Urological Association in 2022 setting a new goal of 80% In 2010, only 6% of patients qualified for AS opted for this approach.
Several European countries and the state of Michigan’s MUSIC (Michigan Urological Surgery Improvement Collaborative) program have reached AS uptakes of around 90% or higher.
Panel members will present their stories followed by a discussion and a Q&A involving the audience.
The panel includes:
--Dr. Mats Steinholtz Ahlberg, consultant urologist at Uppsala University Hospital in Sweden, is involved in major research on active surveillance in Scandinavia and the United Kingdom. Sweden has among the highest AS rates in the world, well above 90%. Ahlberg is involved in research on AS as a doctoral student at the department of surgical sciences at Uppsala University.
--Dr. Chris Bangma, professor of urology at Erasmus Medical Center in Rotterdam, is a leader in the introduction of active surveillance in Europe. He is the coordinator of PRIAS and GAP3 studies.
--Dr. Kevin Ginsburg, of Wayne State University in Detroit, and a prostate cancer leader in MUSIC (Michigan Urological Surgery Improvement Collaborative), which has achieved America’s highest AS rates for men with low-risk prostate cancer (91% vs. 60% nationally ) and also favorable intermediate-risk prostate cancer (45% vs. 20% nationally).
--Professor Vincent J Gnanapragasam, Professor of Urology at the University of Cambridge and Honorary Consultant urologist, U.K., will present the Prostate Predict algorithm which provides personalized estimates of the likelihood of prostate cancer death versus other causes of death over a 10-15-year period after a man is newly diagnosed. Dr. Gnanapragasam believes that the use of such algorithms is the key to increasing AS uptake and reducing variation in the information men are given on the value of radical treatment.
The Active Surveillance Coalition includes Active Surveillance Patients International (ASPI), the AnCan Virtual Support Group for Active Surveillance, Prostate Cancer Support Canada, Prostate Cancer Research Institute, and TheActiveSurveillor.com newsletter. Europa Uomo, the European confederation of prostate cancer groups, the Prostate Forum of Orange County, and the Walnut Foundation in Toronto have endorsed this webinar.
AS 101 News
Dr. Laurence Klotz, the “father” of Active Surveillance, is featured in the second video in the series “Active Surveillance 101” which will be presented at the Active Surveillance Patients International (ASPI) meeting at 12 p.m. ET on Oct. 29.
Register here.
AS 101 is a series of conversations between actual patients and their partners/spouses and leading prostate cancer experts covering essential questions.
The goal of this series is to reach all AS candidates, including those who have not yet been diagnosed with prostate cancer but have rising PSAs (prostate-specific antigen) blood levels to provide them with an introduction to AS.
We—The Active Surveillor was one of the organizers—want to provide the tools to help these patients formulate questions when they go to their family doctors, urologists, or oncologists.
(Nancy and Larry White, spouse/patient meet with Dr. Klotz in AS 101 video)
AS 101 also is aimed at newly diagnosed patients on AS and established AS patients who want a refresher.
The premiere of part 1 of AS 101 has just aired at the monthly meeting of ASPI to view.
The video features a patient and spouse, Larry and Nancy White, a real couple from New Mexico, meeting with family doctor Dr. Stephen Spann, dean of the University of Houston College of Medicine, on a consultation about rising PSA, treatment options, and a referral to a urologist. The prostate cancer “journey” often begins in the office of a primary care physician like Spann to discuss rising PSAs and then moves on to other specialists, such as urologists like Klotz.
The ASPI program includes the video and a question-and-answer period with patients.
In part 2, the Whites meet with Dr. Klotz, who explains early-stage, low-risk prostate cancer. Again, there will be a Q&A.
Earlier this year, ASPI honored Klotz, of the University of Toronto, as the winner of the first Gerald Chodak Active Surveillance Pioneer Award. The late Dr. Chodak was Klotz’s mentor and also was ASPI’s first medical advisor.
In the new video, Larry White, a real prostate cancer patient and himself a physician, and his wife Nancy, who has been an AS advocate, interact with Klotz as in a simulation of a real patient-partner-physician visit.
AS 101 was created under the banner of the Active Surveillance Coalition, whose members include ASPI, AnCan’s Virtual Support Group for Active Surveillance, Prostate Cancer Support Canada, Prostate Cancer Research Institute and The Active Surveillor newsletter.
For more background on AS 101, go to the blog for the Society for Participatory Medicine.
The Active Surveillor is a reader-supported publication. To receive new posts and support my work, consider becoming a free or paid subscriber.














In regard to the one study that reported on anxiety being a determinant for leaving AS at 9%, I would suggest that progression and rising PSA cause anxiety and can lead to a rushed decision to leave AS.
As long as I can recall, Peter Carroll has always maintained that his UCSF cohort shows APPROXIMATELY 1/3 of men remain on AS, 1/3 of men progress, and 1/3 of men opt for treatment.
Frankly that is hardly differnt to what you report here - so Imaybe there is no radical change - 64% to 66%??
The 50% JH number does need some explanation since it shows a lower number opting for treatment - or cnversely a higher number remaining on AS. Does this report those who fell out the study for any reason?