Down the rabbit hole with Active Surveillance
Breaking news: Dr. Stacy Loeb joins the lineup at TheActiveSurveillor.com
By Howard Wolinsky
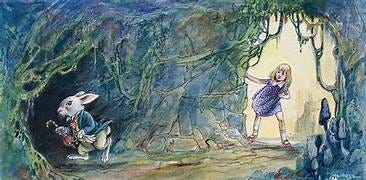
Going on Active Surveillance (AS) for low-risk prostate cancer can feel a bit like Alice’s Adventures in Wonderland, falling down the rabbit hole and tripping into a bizarre, disorienting alternate reality.
We’re told we can co-exist for a long time, maybe until something else kills us, with our cancers, contrary to advice we always heard about cancer. Friends and family may think we’re nuts if we drink this Kool-Aid.
Not everybody believes. 40% of men diagnosed with low-risk prostate cancer in the United States still opt for radical surgery or radiation and accept the risks for urinary incontinence and erectile disorder. (Back in 2010 when I was diagnosed, 94% of men with low-risk prostate cancer opted to undergo aggressive treatment. So things have evolved.)
I have encountered a few rather distinguished rabbits who warn that urologists are putting too many of us on AS. (Do they keep staring at their pocket watches because they have to hurry to see their next patient?)
One of the more controversial ones is Dr. E. David Crawford, professor of surgery and radiation oncology, head of the Section of Urologic Oncology at the University of Colorado Denver School of Medicine, and associate director of the University of Colorado Comprehensive Cancer Center.
I have interviewed him several times for TheActiveSurveillor.com and for MedPage Today. I like him because he’s a straight shooter and because he challenges the conventional wisdom.
He told me that as a man with very low-risk prostate cancer, I probably should never have gone on AS to begin with. I can’t turn the clock back.
(My microscopic “cancer” was seen once in a single core in a biopsy in 2010 and never again in five other biopsies. All but one of these biopsies were done back when annual biopsies were routine. Of course, that’s my story and not necessarily yours.)
In OncLive, Crawford takes the position that too many of us are going on AS. He said some urologists are making an effort to minimize the number of individuals placed on AS.
Crawford told me in MedPage Today [free subscription required] that PSA used along with molecular testing can help many men stay off routine PSA for perhaps 5 to 10 years before repeating it, modeling it after colonoscopies. He said his approach will save many men from biopsies, which carry risks of sepsis and other infections and also spare them years of worry from anxious surveillance.
(Dr. E. David Crawford)
Crawford would keep many men with low PSAs away from annual PSAs and would keep monitoring men at the highest risk for aggressive prostate cancer. Crawford has suggested a new cutoff of 1.5 ng/mL vs. the traditional PSA cutoff of 4 to sound the alarm.
"I picked that cutoff because when you start going above that you do have a risk of prostate cancer that is significant. And if you let it get above a cutoff of 4, you'll find more cancers but you'll also miss some bad ones that might have been found earlier," he said.
Crawford said in OncLive “for those under surveillance, a commitment must be made to diligently monitor their condition due to the likelihood that approximately one-third of these patients may harbor a more aggressive condition.
He noted that over a 10-year period, a considerable portion of individuals on active surveillance ultimately undergo treatment. I reported last year that nearly two-thirds leave AS within 10 years of being diagnosed, and the majority don’t leave AS because their cancer has progressed. PSA prison, anxious surveillance, AS exhaustion, and other reasons can lead men to leave AS Wonderland.
Crawford said that biomarkers can be used for enhanced monitoring to spare men from unnecessary biopsies. [Check out Crawford’s website at www.pcmarkers.com.] He notes that in general urologists have shifted men away from annual biopsies.
Some AS programs recommend three to five years between biopsies and greater reliance on magnet resonance imaging to sniff out potentially aggressive tumors and deliberately overlook smaller lesions that most likely won’t become aggressive. (If they eventually do become aggressive, there is plenty of time for treatment.)
Crawford said frequent biopsies may not always be necessary. Instead, certain triggers, such as a rise in PSA levels or the emergence of new urinary symptoms, could prompt the need for biopsies according to established guidelines, he said.
Discuss any of this with your own urologist before making any changes. AS can seem like Wonderland but most of you can fare quite well and avoid unnecessary treatments with serious side effects.
Coming soon: Dr. Stacy Loeb on lifestyles and active surveillance
By Howard Wolinsky
Many of you already have responded to the new feature in TheActiveSurveillor in which you ask experts in urology (Dr. Michael Leapman of Yale), radiology (Dr. Antonio Westphalen of University of Washington), pathology (Dr. Ming Zhou of Tufts) and sexual health (Dr. Anne Katz, author and clinical nurse specialist at the Manitoba Prostate Centre).
Big news: Dr. Stacy Loeb, a urologist and lifestyle medicine expert, is joining the line-up to take questions about diet, exercise, sleep, and Active Surveillance.
Send your questions to mailto:pros8canswers@gmail.com.
Please keep your questions short and sweet. Tell us a little bit about you, including age, where you are from, when were you diagnosed, lesions, PSA, PI-RADS, etc. Sign with your name and a signature, such as “Forlorn in Flossmoor” or “Puzzled in Pittsburgh.”
TheActiveSurveillor.com is thrilled to have Dr. Loeb on board.
Dr. Loeb is a Professor of Urology and Population Health at the New York University School of Medicine and the Manhattan Veterans Affairs Medical Center. She is a Board-certified urologist, specializing in prostate cancer and men’s health. Dr. Loeb has had more than 400 peer-reviewed publications and received multiple grants from the Department of Defense and National Cancer Institutes for her prostate cancer research. She hosts the Men’s Health Show on SiriusXM satellite radio channel 110 on Wednesdays from 6-8pm ET, and also frequently posts about prostate cancer on X (formerly Twitter) (@LoebStacy).
Check out the inaugural column with Yale’s Dr. Michael Leapman:
Yale urologic oncologist Michael Leapman covers PSA density in new column
[Editor’s note: This month, TheActiveSurveillor.com inaugurates four columns from experts responding to questions about Active Surveillance (AS) and lower-risk prostate cancer. Our leadoff hitter is Dr. Michael Leapman, a urologic oncologist from Yale [Go Bulldogs/Handsome Dan]. Send your questions about AS and urology, radiology, pathology, and sexual…







Ken,
The guidelines don't necessarily say.
But if your PSA is rising on AS--rather than rush into a biopsy, you should have an MRI. MRI is good at finding the more dangerous larger lesions but lousy at finding the smaller ones that may never be a problem or for which you can your time and monitor.
Fewer than 50% of docs things that way, but I am assured that its the standard now.
There is a debate on when to escalte--should it be a PSa of 1, 1.5 or the traditional 4. PSAs are supposed to be great for more advanced cancers, but can be confusing since patients with very low or very high PSAs may hace cancer, That's Dr. Crawford pushes biomarker testing, which can be a beacon on whether to have a biopsy..
Yes, the communicatiopns are confusing for both prostate and breast cancers.
Thanks, Steve,
My goal here is for people to speak out and discuss amongst themnelves.
Like Hyde Park in London. No Gods. Just us Alices, confused and curious and finding our ways as strangers in a strange land.
Howard