Dr. Scholz: Things have improved in 13 years, but 'prostate snatchers' still lurking out there
By Howard Wolinsky
In August 2010, Mark Scholz, MD, and his patient Ralph Blum sounded the alarm about overdiagnosis and overtreatment of prostate cancer in their expose “Invasion of the Prostate Snatchers.”
The Snatchers are still at it.
Later that year, their book helped save me from going under the knife when a urologist told me I had “CANCER!” and promised to “cure” me the following week in his OR. I went on active surveillance, and as I approach my pros mitzvah, have never looked back.
The book has helped thousands of other men. It came out in an updated edition in 2021. Here’s my review.
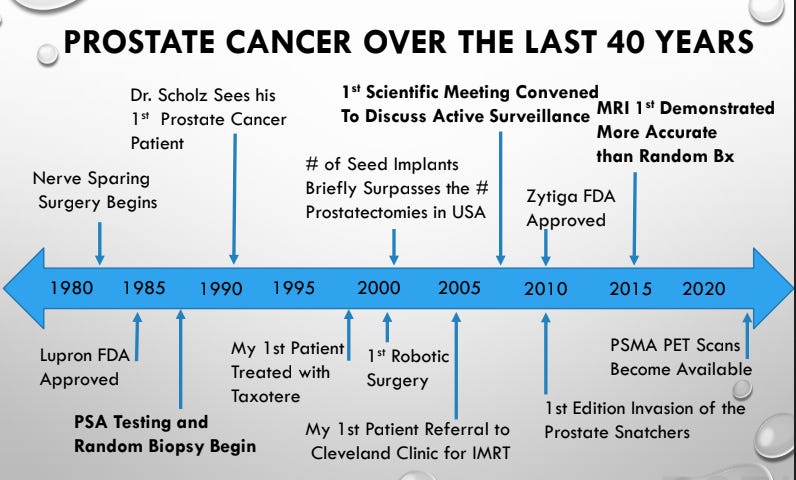
Scholz, of the Prostate Cancer Research Institute in Marina del Rey, California, told a webinar on Jan. 30, 2023, “Invasion of the Prostate Snatchers: 13 years later,” hosted by AnCan Foundation with a record-setting registration of nearly 1,000, that many things have changed in the past 13 years regarding prostate cancer—such as greater enrollment in Active Surveillance, availability. of mpMRIs, fusion biopsies, improved radiation therapy—but the “prostate snatchers” are still lurking out there.
This is evidenced by the numbers: About 6% of patients eligible for AS actually went on in 2010 with the number growing to 60% in 2021. But that means 40% of patients are opting for aggressive surgery and radiation, per the American Urological Association AQUA database.
“Many things have changed in the last 13 years. But the underlying message has not changed. The underlying message is that what people initially think they know about cancer when they're informed of any cancer, particularly a prostate cancer diagnosis is often grossly inaccurate based on how much has changed in the last 10-15 years,” he said. “The amount of knowledge we have has exploded. And you want to be well-informed about the latest things in medicine, because much of it is very, very good news.”
Scholz said the word “cancer” may be frightening to patients. “It's so important to help people understand that the word cancer doesn't really say much, because you can have skin cancers that are harmless. And you can have leukemias that are very, very dangerous and everything in between. So if someone says they have cancer, we have to dig down deeper and find out what does it really mean? And it's such a frightening word though many times people don't get past that.
“So colon and prostate cancer are both serious diagnoses in many men. Colon cancer and prostate cancer are killing about the same number of people every year, but if you look at the annual number of cases that are diagnosed, you can see that the ratio of people dying to diagnosis is about one-eighth of people diagnosed are at risk for dying of it.
“The time for someone to have their day of reckoning, where actual mortality occurs can be on average about 13 months after a failure for colon surgery, but averages about 13 years after a failure for prostate surgery. So we're talking about a condition that can slowly over a period of many years be deadly, but the long timeline of prostate cancer is so distinct from other cancers that it makes it hard for people to wrap their heads around it and adapt to these realities, especially since this is a condition occurring in elderly men to start with.”
He contrasted prostate cancer with lung cancer, pancreas cancer, bone cancer, and brain cancer.
“Why are these other cancers so much more deadly than prostate cancer is? They grow far more quickly. They metastasize. And that word metastasize is really the crux of what makes cancer dangerous. They metastasize much more easily than prostate cancer does. And when they spread, they spread to critical organs such as the liver, lung and brain, which you really can't afford malfunction of, whereas with prostate, lymph nodes and bones are very tolerant and can endure actually quite a few metastases without malfunctioning,” Scholz said.
“With all these other cancers, pancreas cancer, bone cancers, lung cancers, there's no such thing as hormone therapy. With prostate cancer, the median response time of relapsed prostate cancer after surgery or radiation with modern up-to-date hormone therapy is 18 years. Yes, I said that correctly: Median response, average response time to keep the PSA in check. I'm talking about living 18 years. I'm talking about being in remission 18 years. How can this be? Well, one reason is hormone therapy is effective, but the other reason is that we catch prostate cancer recurrences much earlier because of PSA.”
Scholz is an unusual player in the prostate cancer world. He’s not a urologist or a radiation oncologist but a rare medical oncologist focused on prostate cancer. That’s why so many patients gravitate to his practice.
(Go to https://pcri.org/ to find out about his upcoming webinar on PSMA PET, proton therapy and advanced treatments. PCRI’s fall conference will focus on Active Surveillance.)
Scholz said, “There's all different levels of medical doctors. And none of them are out there saying, ‘I don't know what I'm doing.’ They're all saying I know what I'm doing, follow me. And some of them are doing it with relatively little experience. So you have to be careful in that department. And I think support groups are a wonderful way to learn about the good doctors in your community.”
“One of the challenges is finding experts that are really on the cutting edge.”
Scholz said more advanced prostate cancer patients benefitted over the past two years from a new test PSMA (Prostate-Specific Membrane Antigen) PET scanning.
(See Richard Maye’s take in TheACtiveSurveillor.com on getting a PSMA PET as patient with Gleason 3+4. Note: This test is hard to get unless you have advanced cancers and difficult to persuade Medicare to cover. PSMA PET not available for Gleason 6 patients.)
Scholz said really what differentiates a harmless prostate cancer from a dangerous one is metastasis, the spread outside the gland.
“So, the stage of the tumor itself has rocketed to the number one position now that we have PSMA PETscans,” he said. “In the past, we had to use the Gleason score … to try and guess about the possibility of metastatic disease because bone scans and CAT scans needed a chunk of cancer that big before they would show up on a scan. Now, with PSMA pet scans, two-millimeter lesions will light up brightly on a scan. So instead of guessing about whethert he cancer has spread, we actually can do a scan and find out if it has spread.
“So tumor stage as judged by PSMA pet scan, in my opinion, has now become the new most important metric. Whereas in the past, … the Gleason score was the best way to predict the likelihood that cancer was outside the prostate because whether it's outside the prostate or not is ultimately the most important determinant.”
He said the second most important thing is still the grade or the Gleason score, and there's genetic testing (Decipher, Oncotype Dx, and Prolaris). “The third most important factor, and these are in a hierarchy of relevance, is the size of the tumor. That has to do with how big it is on a scan, say an MRI or an ultrasound, percentage of cores positive on a random biopsy,” he said. “I'm not a fan of random biopsies, but they're still happening and the PSA. High PSAs have argued for larger amounts of cancer, lower PSAs for smaller cancers.”
“One of the biggest problems that I see in the prostate cancer world, not only for patients but also for doctors, is an absence of perspective, a lack of experience about how diverse prostate cancer is. And to understand what to do and where a person stands, there has to be an understanding of how this particular disease fits in the spectrum of all the other prostate cancers.
“We know a lot about prostate cancer, but we don't necessarily know how to identify where a specific patient fits in that spectrum. Clearly, if the disease is more aggressive, we want to use more aggressive treatment. And if the disease is less aggressive, we want to use milder treatment, obvious, but sometimes lost in the shuffle of the complexities and all the fears that people are enduring with us.”
Scholz said PSMA PETnoffers the potential to radically change prostate cancer treatment.
“With the advent of PSMA PET scans, we are starting to consider cutting back on hormone therapy, testosterone blockade, androgen deprivation, because these hormone treatments are designed to provide insurance against the possibility of micrometastatic disease. But now with PSMA pet scans, are we in an era where we can forego hormone therapy when we don't find any metastatic disease? There are no studies yet to address these questions. But it's very logical to consider pulling back on hormone treatment, which can be administered for six months in an intermediate-risk patient, 18 months in a high-risk patient. Certainly effective in people with proven spread, but in people without any metastasis as per PSMA pet scans. Can we think about skipping the hormone treatment?”
Scholz said patients come to him because they are confused when a radiation oncologist recommends radiation and a urologist recommends a radical prostatectomy.
***
Active surveillance may not have even been put on the table for discussion.
“Pretty sad that that's the the way that modern prostate cancer is looked at when we have a spectrum of options for people now,” he said.
He said doctors and patients historically have relied on the Gleason score as the most powerful indication of whether the cancer would spread. And there's a lot of confusion about the grade of prostate cancer.
“Gleason 6 prostate cancer has never been shown to metastasize. It's a harmless benign tumor that stays inside the prostate. So, this is about half of the men -- of the 200,000 men diagnosed every year, about 100,000 have Gleason 6. So 100,000 men should be considering watchful waiting or active surveillance as their primary treatment program,” he said.
“Gleason 6 is almost like normal prostate tissue,” he said. “You start to lose some of that architecture in the Gleason 7, but it still retains some of its desire to act like a prostate gland. But when you get into the Gleason 8s through 10s, we lose most of that architecture. And it's mostly just cells. And this is something that wants to behave more like a cancer than like a prostate gland. And the statistical possibility of spread goes up.”
***
Scholz long has been a critic of random biopsies as opposed to fusion biopsies that focus on lesions found in an MRI.
“Random biopsy is still incredibly popular. And over a million(American) men go through this every year. One of the other problems is not infections, not the discomfort, but the fact that we find more Gleason 6 cancer, and since people hear the word cancer about a third of men that are diagnosed with Gleason 6 are still talked into unnecessary radical surgery or radiation. And that's about 30,000-40,000 men a year that are undergoing treatment for something that does not require treatment. That's a big deal, and that's largely due to the problems with random biopsy, finding little specks of grade six around the prostate.”
He said high PSAs should be examined with an MRI not a random biopsy. “MRIs that show higher grade lesions -- if they see shadows on an MRI they'll grade them from 1 to 5. And 4s and 5s should have a targeted biopsy of the lesion. It's rather simple idea. Patients get it very quickly, but the industry has been very slow to adopt this technology.”
He said, “Targeted biopsies work.”
Scholz described a recent European study found that out of about 9,000 men, only 10 men on the random biopsy that were not picked up by the targeted biopsy with what was called clinically significant prostate cancer. “This means it was not pure 3+3. It was 3+4. All 10 of these 3+4s were small and were felt to be appropriate for management with active surveillance,” he said. “They did not find anyone with only random biopsy alone in this huge study that needed to go onto radical therapy, rather amazing.”
I have asked Scholz about renaming Gleason 6 as a noncancer.
Here’s his response: “The word ‘cancer’ has technical implications in the medical world that are related to its cellular appearance under the microscope and its capacity for unregulated growth. The same word ‘cancer’ has a quite different and very clear meaning to the general public—it means ‘metastases and death.’
”Close to 100,000 men in the US are terrified every year when informed that they have ‘Grade 6 prostate cancer’—a condition that has been proven to have zero metastatic potential.
”I entreat the powerful medical-industrial complex that makes billions of dollars every year treating prostate cancer to have a heart, to have mercy on the uninformed public, and stop calling this harmless entity ‘cancer.’”
Alex Scholz, CEO, of Prostate Cancer Research Institute, recently shared my AS story. More than 5,000 people have viewed it. How about you?







Martin, I am not sure of the citation. I will ask. Howard
Part I:
1) Re your citation from Dr. Scholz: "Scholz described a recent European study......." could you provide a link to that study, since most recent studies out of Europe and the U.S. conclude that the combined MRI-Targeted and Fusion/Systematic biopsy is more efficacious than an MRI-Target biopsy alone. The overall estimated false negative rate of mpMRI is around 10–20%. I believe that biopsy is the standard of care at Johns Hopkins with a large AS cohort.
2) Dr. Scholz incorrectly refers to the systematic portion of the combination biopsy as "random." It is not.
3) You refer to statistics per the AUA Aqua Database. A recent study, among the authors of which are Cooperberg and Catalona can be found here: https://jamanetwork.com/journals/jamanetworkopen/fullarticle/2801916
I cite it because I think patients would benefit from reading the entire study including the section with the header: Limitations. In that section, the authors state "Our definition of AS is intentionally liberal; follow-up with PSA testing alone without subsequent biopsies is not considered adequate AS but has been documented very commonly in community practice," citing a Michigan study.
4) In your article, you refer to the "Oncotype, Polaris and Decipher" tests. In his January 30 webinar, Dr. Scholz advised patients to avoid the Decipher test.
In my opinion, Dr. Scholz's book was groundbreaking and was instrumental in moving the needle on unnecessary over treatment and towards Active Surveillance. There is no doubt about that. However, now, work needs to be done to bridge the divide in the PCa community, as to how to communicate diagnoses of low to favorable-risk cancer to patients. The premise that there are "more prostate snatchers" out there serves to fan the flames of the divide.