By Jeffrey Coleman
“Absolutely.”
This was the response he gave me to my question. Without hesitation.
No “hmmmm.” No “well, maybe.”
And this was the response I was hoping to get, but hearing it expressed with such certainty made the answer all the more gratifying. My wife Theresa and I looked at each other with big smiles!
But who was “he” and what was “my question”?
First, a bit of history.
From 2018 through 2020 I had rising PSA levels each year (3.7 / 4.6 / 4.9). In June of 2020, I decided to see a urologist. At that time, I was 60 years old. I chose to go to Johns Hopkins, a local “center of excellence” in Baltimore, Maryland, which is thirty minutes from my home. My PSA test there came up again as 4.9. There was nothing felt by the doctor on the DRE. He recommended an MRI followed up by a biopsy.
The results of the mpMRI (3 Tesla / with and without contrast) showed a small lesion within the prostate designated as a PIRADS 3 (equivocal / may or may not be cancer).
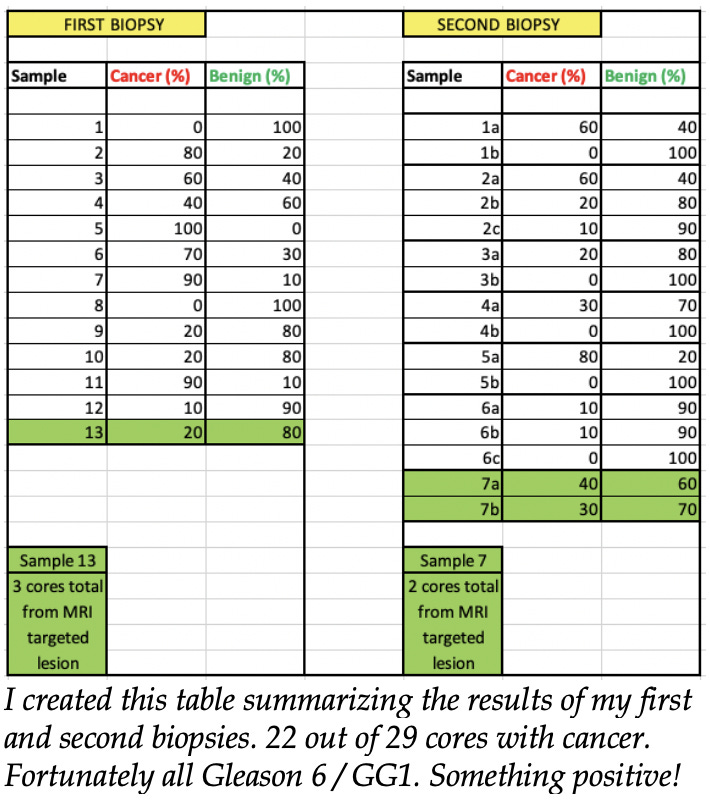
I had a transperineal biopsy in September 2020. Three cores were taken from the MRI-targeted lesion along with another 12-core systematic sampling. Three days later, the urologist called. He gave me the famous “good news / bad news” scenario. The “good news” was that of the cancer found, it was all Gleason 3+3=6 (GG1). The “bad news” was that I had “high volume.” He described this as numerous cores containing cancer.
I was certainly stunned by this news, but being pragmatic, almost to a fault, I asked him straight away what was our next step. Right away, he said, “radical prostatectomy.” Right away, I said, “Ain’t happening!” By this point in my journey, I knew what that was and knew of the serious side effects associated with the surgery.
I asked about another option I had heard of called active surveillance. He said if I was interested in that, he could give me the name of the doctor at Hopkins who was the head of the AS program. I got the name of that doctor and set up an appointment with him. Also, at this time, I got a second opinion on my pathology report from the famed pathologist Dr. Jonathan Epstein at Hopkins. He concurred with the original pathology report.
I had a Zoom appointment with the Hopkins AS program head in October. We discussed my situation. He described my cancer as “unusually widespread, high-volume Gleason 6/GG1.” There was that “high-volume” term again. His opinion was that “high volume” was having three or more cores that have greater than 50% cancer. He felt I should be treated, if not with RP, then perhaps something like TULSA (Transurethral ULtraSound Ablation). His opinion was that high volume could be indicative of more aggressive cancer that wasn’t found or potential of upgrading in the future. However, he was willing to put me on AS. We would monitor my PSA, get another MRI, and another ”confirmatory” biopsy in 12-18 months. My wife was and still is completely supportive of my decision.
I had a second biopsy in May of 2022. This was also transperineal, with two cores targeting the MRI lesion along with a 12-core systematic sampling. Again the results showed a high volume of all Gleason 6/GG1, although this time aggregately less cancer. Again, Dr. Epstein concurred via a second opinion.
During the post-second biopsy consultation with my doctor, he again felt I should consider treatment. I told him I would prefer to stay on AS at this time. He was willing to defer to my decision, and we would continue to monitor via MRIs and PSA tests.
So for almost three years now, I have been on active surveillance. This was the only option I would allow myself at this time. I am relatively young. I am otherwise very healthy and active. I, in no way, wanted to deal with the side effects of any type of treatment and how they would affect my lifestyle. Yet, although being on AS was my choice, there were numerous times when I wondered if I was playing with fire. Was I taking too big of a risk because of having “high-volume” Gleason 6 / GG1
I tried to learn as much as I could about PCa and AS by reading research studies and articles along with watching webinars from some of the leading urologists in the field. There was certainly a lot of information to wade through. Below are some points I took note of:
—I could find no concrete number to define what high volume is. My doctor said three or more cores that have greater than 50% cancer. Some studies said more than four cores with cancer, but that was just the criteria for that study. My thought had always been there should be various levels of volume stratification to help aid in risk assessment. Ultimately though, even with no real definitive “number” for high volume, I have it.
—Some doctors (including my own) say high volume can indicate more aggressive cancer not found via MRI or biopsy. However, this is what they say generally regarding MRIs and biopsies. MRIs can miss small tumors and are also subject to the expertise of the radiologist interpreting the images. Targeted biopsies combined with twelve systematic cores only sample a very tiny percentage of your overall prostate. Something worse could have been missed.
—I was told high volume may increase the chance of grade progression over time. My thought was why would high-volume Gleason 6/GG1 be more likely to progress? Gleason 6/GG1 is Gleason 6/GG1 no matter the quantity.
With that said numerous studies I’ve read and webinars I’ve seen have experts playing down the aggressiveness of Gleason 6/GG1. This caught my attention. I took particular notice of this topic being discussed by two prominent urologists, Dr. Laurence Klotz of UToronto and Dr. Scott Eggener of UChicago.
Dr. Klotz is considered one of, if not the “father of active surveillance.” He has stated that Gleason 6/GG1 never metastasizes. Dr. Eggener has said he is convinced that no man has ever died from “pure” Gleason 6/GG1 prostate cancer. He is now at the forefront of a movement to have Gleason6/GG1 no longer labeled as cancer.
I started to wonder what these two doctors might have to say about my case. Yes, I have all Gleason 6/GG1 but would a “high volume” of it possibly make them wary of me being on active surveillance?
And so this brings us back to the beginning of this article, where I wrote:
But who was “he” and what was “my question”?
“He” was Dr. Laurence Klotz. “My question” was would he put me on active surveillance if I was his patient? And without hesitation, he said, “Absolutely.”
I decided to get more opinions on my case. I chose Dr. Klotz because of his vast experience in the field of active surveillance. I knew he was certainly a huge proponent of it but what about my situation? What about this “high-volume” Gleason 6/GG1? I didn’t choose him with the expectation of him recommending AS because that’s what I wanted to hear. I actually chose him with the thought that he might possibly not recommend it in my case. I wanted to see if he thought my case was too severe for AS no matter how much he is an advocate for that option.
Some brief bullet points from our discussion:
He has many men in his practice with high-volume Gleason 6 on AS
Studies have shown chance of aggressive cancer is almost zero
Chance of metastasizing is almost zero
Chance of becoming locally advanced (outside the prostate capsule) maybe 2%
1.5% per year upgrade /progression from Gleason 3+3, and that would be to Gleason 3+4 which can still be considered favorable for AS
His expectation: I would never need treatment, or it would be far in the future
So this was all very reassuring to hear! I was very grateful for Dr. Klotz consulting with me. He was extremely cordial and at no time did I ever feel rushed.
Am I done getting more opinions? Not sure. I think I would like to hear what Dr. Eggener’s opinion would be of someone with all “non-cancer” but a “high volume” of it.
After all, isn’t it in all of our best interests to advocate for ourselves when it comes to dealing with our disease? We all know the answer to that question. Without hesitation.
“Absolutely.”
Jeff Coleman, 63, lives in Eldersburg, Maryland. Born in Johnstown, Pennslyvania, he says he will always consider himself a Pennsylvanian at heart (Go Steelers!) He recently retired from Verizon after 33.5 years on the job. Most recently, he was Fiber Facility Provisioning Coordinator. (Don’t eat this sort of fiber, please.)
Jeff enjoys traveling. He recently returned from three weeks in The Netherlands and Belgium. He and Thersa also planning more extensive domestic travel,
He rides a motorcycle, currently a 2022 Triumph Bonneville. He enjoys fly fishing for trout. He and Theresa kayak and ride bikes.
He is a huge American Revolution history buff.
Who are his favorite Revolutionary War figures? “Interestingly enough, I have kind of a soft spot for Casimir Pulaski, who you guys in Illinois actually celebrate in March—a Polish immigrant who gave his life for ‘The Cause.’
“Believe it or not, I do have a bit of empathy for Benedict Arnold. An interesting story when read into more deeply.”
The Colemans have a 28-year-old son Nathan, an assistant superintendent for a large commercial concrete company out of Frederick, Maryland.
TheActiveSurveillor.com featured Jeff in May 2022 in a series on perineural invasion:
(Part I)Perineural invasion: Not so scary
By Howard Wolinsky In 2020, Jeff Coleman, 62, of Eldersburg, Maryland, outside of Baltimore, was diagnosed with high-volume Gleason 3+3=6 prostate cancer. “There was some initial discussion with my doctor about treatment due to the high volume but we both ultimately agreed on Active Surveillance. PSA tests during AS (3.9 and 4.1) were lower than my highes…
I’m going back to college
By Howard Wolinsky
I wanted to share some personal news with you.
I have been accepted for the Master of Public Health program at the University of Illinois at Chicago School of Public Health. I start in late August.
I increasingly have been involved in research on prostate cancer and also heart disease and breast cancer in a variety of ways, with CDC and several major universities as well as patient-centered research.
Dr. Scott Eggener, my former urologist, pulled my leg by saying I had begun my academic career in my mid-70s. (I gather he doesn't count the decade I taught medical journalism to grad students at Northwestern's Medill School as well as UChicago and DePaul.)
Also, I am interested in health policy analysis, a focus in the MPH program, along with research methods.
I think the work on an MPH will put me a better position to work on prostate cancer issues. I am open to whatever doors might open.
My application essay was entitled, "Why I want to get a MPH before I turn 80." Son David calls me “college boy.” He ran my essay through AI and got a hilarious take on my application from the viewpoint of Beavis and Butthead.
UIC placed me in an "enhanced" program, which requires six fewer credit hours than the regular MPH. I get credit for life experience.
The American Public Health Association back in the early 1970s honored me as "the best young science writer" in the US. Now, I may be one of the older candidates for a public health degree.
I don't know yet what the demands of these studies will be. Something may have to give. I am not sure what.
Check this out for a laugh: https://tinyurl.com/579358t6. Beavis & Butt-head offer an opinion on my adventure
Stay tuned. Get a paid subscription and help my scholarship fund?
ASPI on July 1: ‘Pissed Off: The Many Ways Urination Can Go Wrong’
By Howard Wolinsky
Dean Elterman, MD, an academic urologist at the University of Toronto, is presenting a free webinar, “Pissed Off: The Many Ways Urination Can Go Wrong” to Active Surveillance Patients International at 12-1:30 p.m. Eastern on July 1, 2023.
Click here to register: https://tinyurl.com/5d7ypd8k
He’ll cover the waterfront of topics, from BPH to incontinence to overactive bladder.
The session will be followed with a live Q&A.
(Dean Elterman, MD, University of Toronto.)
Elterman’s research interests include voiding dysfunction, benign prostate enlargement, and men’s health.
He is the medical director of the Prostate Cancer Rehabilitation Clinic at Princess Margaret Cancer Centre in Toronto.






Jeffrey mad a wise decision in my opinion by standing his ground and not jumping into surgery. If his urologist that wanted to do surgery believes that his case is that dire, perhaps he could convince the health insurance provider to pay for a PSMA PET scan. That, to me, will provide the answers he needs. Richard M.
i may have missed it but in my view high volume 3=3 should have gentics and a PSMA scan. The hell with the guidlines, in his case all of the information that you can get you should get.