If Gleason 6 were redefined as noncancer, only 5% of patients say they would quit surveillance; 82% would stick with program.
Patients share their views on Gleason 6 in survey
By Howard Wolinsky
Over the past year, urologists and pathologists have been debating whether Gleason 6 lesions should be considered cancers.
Now, a patient-led survey reveals that patients with low-risk prostate cancer, like their urologists, are divided on whether Gleason 6 should be reclassified as a noncancer. Also, the survey shows that patients, by a wide margin, say they would remain on active surveillance (AS) if Gleason 6 lesions were considered noncancers.
The survey will be presented in a poster at the American Society for Clinical Oncology Genitourinary in San Francisco.
Urologists have been split 50-50 on whether this low-risk lesion, which looks like a cancer but doesn’t act like one, should be considered cancer.
Proponents of change say a “pure” Gleason 6 has never in the history of medicine been shown to metastasize or kill. They also say the cancer label causes avoidable emotional distress and financial toxicity to patients.
The vast majority (more than 80%—see article below) of pathologists, the medical umpires armed with microscopes and keen brains who make the call on whether lesions are cancer, want to maintain the status quo. They maintain if a lesion looks like cancer, it should be called cancer. They don’t believe a Gleason 6 can be confirmed as “pure” in a simple biopsy, but only after a radical prostatectomy.
And if Gleason 6 were redefined, the pathologists and many urologists fear that patients will abandon surveillance—close monitoring of lesions with PSA blood levels, digital rectal exams, MRIs, and biopsies—and the window for treatment could be missed if cancers “progress” to more dangerous Gleason scores.
Until now, the people these debates and decisions affect the most—patients like you and me on AS for low-risk lesions based on Gleason 6 scores—haven’t had a say in the matter.
The results of a survey of patients, conducted by AnCan, Active Surveillance Patients International and Prostate Cancer Support Canada plus The Active Surveillor and three prostate doctors will be presented as a poster at ASCO’s Genitourinary Cancers Symposium.
Here’s the bottom line from the survey of more than 450 patients currently or formerly on active surveillance as reported in the poster:
—Patients are just as divided on the Gleason 6 debate as their doctors. 35% each support or oppose reclassifying Gleason 6 as a noncancer. 30% are undecided.
—Despite warnings from most pathologists and many urologists, only 5% of respondents say they would drop surveillance. 83% say they would continue on AS even if they were liberated from a cancer diagnosis. The rest were undecided.
—Many (nearly 60%) of these patients experience anxiety at such times as scheduled prostate exams, when they are having PSA blood levels taken, and while they await the results of MRIs and biopsies, which are part of AS protocols. 10% say they are anxious all the time. Patients call this “anxious surveillance.”
—16% experience insurance discrimination from a Gleason 6 diagnosis taking the form of denial of policies or premium increases. This most commonly impacts term life insurance followed by health insurance. The survey provides the first documentation of this type of financial toxicity.
Urologic oncologist Scott Eggener, vice chair at UChicago Medicine, who has spearheaded the debate to rename Gleason 6, said, “The results from this patient-centered survey are an integral component of the ongoing discussion and debate, highlighting the stress and toxicity that come from a diagnosis of Gleason 6, while also reassuring that a very high proportion of men would continue monitoring even if its name was changed to a pre-cancerous term.”
Uropathologist Ming Zhou, MD, PhD, pathologist-in-chief at Tufts and president of Genitourinary Pathology Society, is a rare pathologist to support renaming Gleason 6. (See story below.)
He said: “I am most encouraged by the finding that the vast majority of the respondents will continue on AS even after the cancer is dropped off the diagnosis.”
Mark Scholz, MD, author of the ground-breaking "The Invasion of the Prostate Snatchers” and the moving force behind the Prostate Cancer Research Institute, said:"Over-treatment of prostate cancer negatively impacts male self-esteem, sexual identity and quality of life. Patients and doctors draw wrong conclusions about the risk of metastases when Gleason 6 is called 'cancer.' This inaccurate and inflammatory nomenclature needs to be changed."
(Eggener, Zhou and Scholz weren’t involved in the survey.)
Johns Hopkins uropathologist Johnathan Epstein, MD, who has led the charge against renaming Gleason 6, responded to the survey finding that most men would remain on AS if the cancer name were dropped: “The survey was answered by men who have been diagnosed with cancer, consider themselves to have cancer, and are consequently undergoing close follow-up on AS. Telling these men if we were now to change the name of their cancer to noncancer is not the same as telling a man on their first biopsy with Gleason 6: ‘You don’t have cancer, but we want you to be followed closely for many years with repeat biopsies, imaging, serum tests, etc.’”
Paper co-author Herbert Geller, PhD, a member of the AnCan board and a patient with advanced prostate cancer who led the survey analysis, noted, “AnCan observed the patient perspective was lacking in the literature, so we took it on ourselves to organize an investigation involving several peer organizations.”
Four patient organizations--AnCan Foundation, Active Surveillance Patients International (ASPI), Prostate Cancer Support Canada, and The Active Surveillor newsletter— over four weeks in October and November 2022 conducted the survey on patient opinions on renaming Gleason 6 and other controversies facing these men. Patients responded via SurveyMonkey.
Minhaj Siddiqui, MD, director of urologic oncology and robotic surgery at the University of Maryland Medical Center and associate professor of surgery at the University of Maryland School of Medicine, said the survey provides meaningful insight from patients on this very active academic debate.
“It was helpful to hear how the patient community seems split three ways between agreement, opposition, and being undecided, which reflects the continued opportunity to raise awareness on this topic,” he said.
Samuel L. Washington III, MD, assistant professor of urology, University of California, San Francisco, and co-author, said, "This survey provides an important patient and patient advocate perspective that is often missed or overshadowed by provider opinions. As the patient remains the individual most impacted, it's important that the voice of these crucial stakeholders frames how we discuss and discuss the issue."
Phil Segal, a co-author and facilitator for Prostate Cancer Support Canada Nationwide AS group, said, “Whether G 6 was renamed (and there is little definite consensus on this by the men surveyed), it is clear that men would follow a generally accepted AS protocol.”
Emotional distress issues receive little attention in the prostate cancer world. Major groups, including ASCO, the National Comprehensive Cancer Network, the American College of Surgeons, and the American Cancer Society recommend that all cancer patients be screened for emotional distress. However, the American Urological Association and the American Society for Radiation Oncology don’t explicitly make this recommendation.
The survey found that more than 90% of respondents said they had not been screened for mental health issues.
Rick Davis, founder of AnCan, said, “The survey confirms that emotional distress is a major overlooked issue and one that professional groups representing the doctors who care for prostate patients should tackle in guidelines and in practice.”
Segal noted that emotional distress often accompanies AS. “Giving emotional distress the attention it deserves would ease the AS journey,” he said.
Mark Lichty, ASPI chair and co-author, said, “This survey lends credence to the patients' voice and elevates the significance of anxiety and quality of life. It should be taken seriously.”
Davis said, “As the debate on Gleason 6 continues, physicians ought to consider what patients are saying and not only address the Gleason 6 question but also find ways of tackling the issues of emotional distress and financial toxicity.”
Background on the debate
By Howard Wolinsky
Urologic oncologist Scott Eggener, MD, vice chair of urology at UChicago Medicine, has led the call for Gleason 6 reform. He organized a group with one other urologic oncologist, one radiation oncologist, one pathologist, one biostatistician, and me (a 13-year veteran patient of AS for very low-grade prostate) to call to redefine Gleason 6 as a noncancer.
I dubbed us the Eggener 6.
We published our arguments in the Journal of Clinical Oncology (JCO): “Low-Grade Prostate Cancer: Time to Stop Calling It Cancer.” The article was the top-mentioned article in the journal in 2022, according to a tweet from JCO.
Urologic pathologist Jonathan Epstein, MD, leading second-opinion provider at Johns Hopkins University, and Adam Kibel, MD, chief of urology at Brigham and Women's Hospital—the Epstein 2—presented a rebuttal, “Renaming Gleason score 6 prostate to noncancer: A flawed idea scientifically and for patient care” in JCO,
I helped spark the new debate in January 2021 in MedPage Today in an article entitled “Is this really cancer?” Click here.
Eggener told me: “The singular origin of the Gleason 6 name change proposal is to minimize unnecessary diagnosis, treatment, and toxicity, which can he treatment-related, emotional, financial, or via life insurance.”
The debate has moved beyond academia and medical publications into the lay media in April 2022 after the Journal of Clinical Oncology published the paper by the Eggener 6 about Gleason 6.
The Fox News Network, LA Times, Chicago Tribune, Chicago Public Radio, Associated Press, and other outlets picked up on the debate.
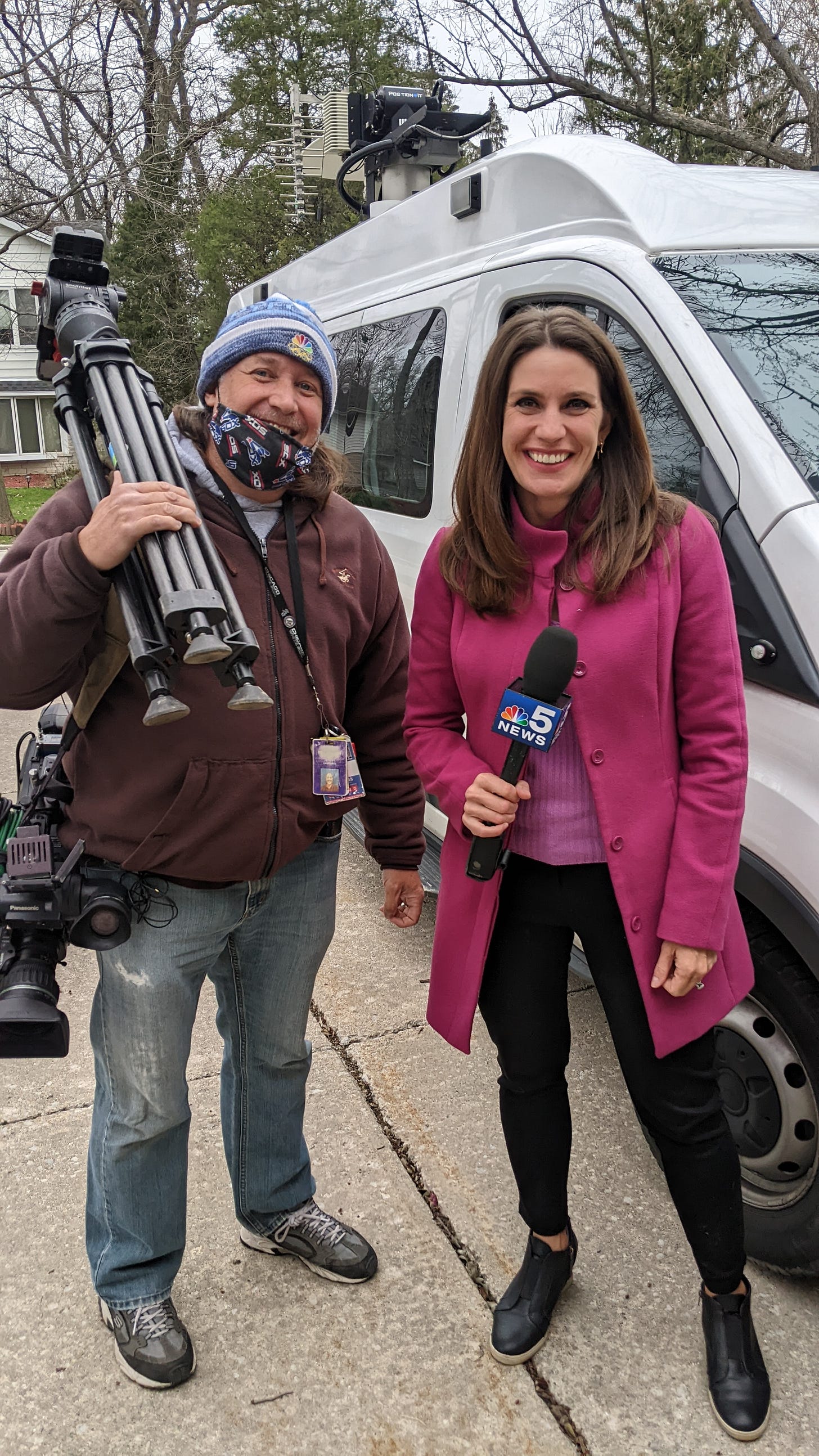
I got my 15 seconds of fame on NBC Chicago. A crew came to my house and interviewed me. Here’s their report.
(Channel 5’s crack reporting team on my driveway.)
(Cimone the cat views the festivities.)
Survey shows: Pathologists ain’t ready for Gleason 6 reform
By Howard Wolinsky
Mathias “Paddy” Bauler, an American saloonkeeper and Chicago alderman, was corrupt, controversial and charismatic Chicago political boss. He’s famous for saying: "Chicago ain't ready for reform yet."
Pathologists generally aren’t either when it comes to renaming Gleason 6 as a noncancer, according to a newly released survey of members of the Genitourinary Pathology Society (GPS).
The survey was published in the February edition of Urologic Oncology: Seminars and Original Investigations.
Ming Zhou, MD, the lead author, is president of GPS, pathologist-in-chief at Tufts Medical Center, and, surprisingly is a proponent of relabeling Gleason 6. (More on that in a moment.)
(Ming Zhou, MD, PhD)
The survey found: Most respondents (196, 81.7%) opposed removing the cancer label from Gleason 6, or GG 1 cancer, 33 (13.8%) supported a change in nomenclature, while 11 (4.6%) responded that they were uncertain. Of those who supported the reclassification, 17 (51.5%) supported the change for radical prostatectomy only, 4 (12.1%) for biopsy only, and 12 (36.4%) for both biopsy and radical prostatectomy.
Zhou et al. said the survey results “highlight the gap between pathologists and clinicians in whether GG 1 prostate cancer should be labeled as ‘noncancer,’ and calls for continued debates and conversations between pathologists and clinicians, and further studies on the biology, diagnostic reproducibility, and ideal management of GG 1 prostate cancer in order to make a more evidence-based decision for patients.”
Urologic oncologist Scott Eggener, MD, of UChicago Medicine, who is leading the campaign to change the status of Gleason 6, said in a tweet that he was heartened by the survey.
He wrote: Good news: 20% willing to consider a change.”
He said: "Current biopsy techniques may not adequately sample cancer and may miss high-grade cancer … do we do this for any other cancer?! Call a non-cancer a cancer based on what isn't on the biopsy?”
Eggener added: "Grade alone does not dictate the biology of GG1: still waiting to hear of the first human in history who had symptoms or mets/death from a pure (only) contemporarily-graded GG1.”
Zhou has been a convert to the position renaming Gleason 6 a noncancer. It hasn’t won him any friends among his fellow uropathologists.
Here’s what happened:
I invited Zhou and Eggener to debate the Gleason 6 issue in summer 2001 in an AnCan webinar. You can watch the two-hour debate here.
A pre-debate poll showed that 55% of respondents thought Gleason 6 is a cancer, while 10% thought it wasn’t a cancer. 35% were unsure.
The numbers changed dramatically after the debate: Only 22% thought Gleason 6 is a cancer, 47% said Gleason 6 is not a cancer, and the remaining 31% were unsure.
Dr. Eggener clearly won the debate.
The following day, something remarkable happened.
Dr. Zhou told me: “Dr. Eggener has won me over. I am now in his camp. I just proposed [to Eggener] to work together to educate pathologists on this topic. As you know, I am also the president of Genitourinary Pathology Society (GUPS, an international GU pathology society). I will do my part to change the name.”
Zhou was risking his political capital as GUPS president to advocate renaming Gleason 6 as a noncancer.
(Scott Eggener, MD)
Zhou told me: “Gleason score 6 (Grade Group 1) prostate cancer meets the pathological criteria for cancer and some of them share molecular features with high-grade prostate cancer. However, it is time for pathologists to seriously consider renaming it as a lesion that will not invoke a strong response typically associated with a cancer diagnosis for the purpose of best management of these patients.”
Zhou said pathologists ought to think beyond just what they see in their microscopes and take a larger view of patient welfare and care.
He expressed the usual reservations about whether would abandon surveillance if Gleason 6 were defined as a noncancer—a point addressed in the patient survey reported on above—and patients miss the window of optimal treatment.
He noted: “However, pathology is not the only factor that determines how these patients will be managed. They will be risk-stratified based on biochemical and molecular markers and imaging. I believe these tests will be able to identify patients at risk for high-grade cancer.”
Zhou should be credited with placing patient care above parochial pathologic definitions. His is a profile in courage.










Thank you Howard, very interesting survey, and I wonder how this question would be experienced in other parts of the world. Is it worth pursuing that?
Sincerely yours,
Prof C.H. Bangma MD, PhD (he/him)
Professor in Urology
Director Anser prostate network
Breaking update: Dr. Jonathan Epstein, the renowned uropathologist, who has led the charge against renaming Gleason 6, could not be reached before deadline. However, he just sent some comments. I included those pertinent to the patient survey in the story body.
Here are his full comments:
"There are multiple reasons why renaming Gleason score 6 to noncancer is flawed scientifically and for patient care as Dr. Adam Kibel and I wrote recently in the Journal of Clinical Oncology September 2022 issue. One of the major arguments against relabeling GG1 as not cancer is that approximately 20%-35% of these tumors on prostate biopsy are upgraded at radical prostatectomy.
"Removing the label of cancer in men with GG1 cancer on biopsy could make it challenging to ensure that they are carefully followed and biopsied sequentially during years of follow-up on AS. Some experts have argued that a recent survey finding that 82% of all respondents say they would continue AS even if the cancer label was dropped.
"The survey was answered by men who have been diagnosed with cancer, consider themselves to have cancer, and are consequently undergoing close follow-up on AS. Telling these men if we were now to change the name of their cancer to noncancer is not the same as telling a man on their first biopsy with Gleason 6: “You don’t have cancer, but we want you to be followed closely for many years with repeat biopsies, imaging, serum tests, etc.”