Stable AS? Past mid-70s? Keep on truckin' on AS. But you can deintensify, deintensify, deintensify--UCSF researchers
(Editor’s note: I was in my mid-70s and had questions about Active Surveillance and what I should do. I discovered, as can be the case often, there were, as I wrote in my column in MedPage Today, no AS guidelines for AS in those of us over 75. Ola Bratt, MD, chairman of the national working group for organized prostate cancer testing in Sweden, which has the highest AS uptake in the world, told me, ‘You raise an important issue. Guidelines are needed for men of all ages.’
(Drs. Peter Carroll, the Active Surveillance pioneer from University of California San Francisco, and Dr. Kevin Shee, his protege and author of The Urology Report column here, started with my question and ran a study, the subject of Kevin’s column below.
(Perplexity rendition.)
(Carroll and Shee concluded it’s worth continuing to monitor low-risk PCa in older patients if they have more than 10-year left on their life horizon at 75 and above. This could bring me into my mid-80s on AS.
(They call for “deintensification”—cutting back on MRIs and fer sure biopsies—as we age. My doctor has been doing that for most of the past 10 years. But I’m still not sure if I want to stick with it. Maybe it’s time for some guidelines from AUA?
(In his 1854 book ‘Walden; or, Life in the Woods,’ philosopher and naturalist Henry David Thoreau expressed the idea ‘simplify, simplify.’
( I just had my first MRI in eight years and am considering next steps. Can I deintensify any more than have—unless I just quit AS/WW? I need to meet with my urologist to discuss further simplication. More to come.—HW)
Question: Can you please describe your motivation behind your most recent AS paper, and why it matters to the Active Surveillance community?
Article: “Determining Long-term Prostate Cancer Outcomes for Active Surveillance Patients Without Early Disease Progression: Implications for Slowing or Stopping Surveillance”
Link: https://pubmed.ncbi.nlm.nih.gov/39341710/
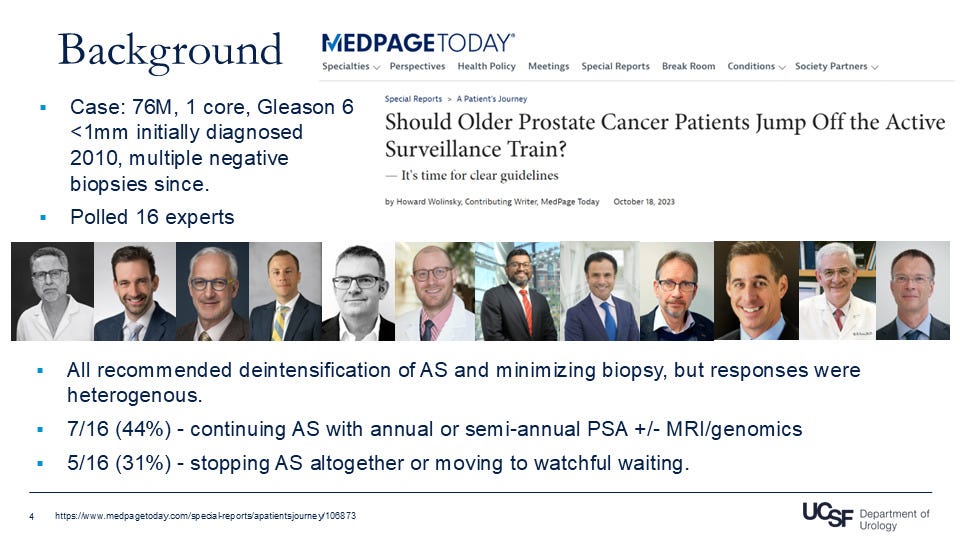
Response: Thank you for the question. The story behind this paper is a fascinating one, and really is a great example of how important the voice of patients and patient advocates are to meaningful research. In this particular case, Dr. Peter Carroll and I happened to come across Howard Wolinsky’s article in Medpage Today: https://www.medpagetoday.com/special-reports/apatientsjourney/106873.
In it, he shared his own story about his diagnosis of Gleason 6 (3+3) prostate cancer and his 5 negative biopsies since while on active surveillance (AS), with PSA of 5 and PSAD of 0.08. He ended up asking 16 prostate cancer experts worldwide about how his case should be managed clinically, and received heterogeneous responses. All recommended some form of deintensification, but the particular protocols differed greatly, from stopping AS to continued monitoring with PSA, MRI, and other testing.
Dr. Carroll and I felt that this article highlighted a currently unmet clinical need—we did a deep dive into the biggest currently available prostate cancer guidelines including the the National Comprehensive Cancer Network (NCCN), American Urological Association (AUA), and European Association of Urologists (EAU), and there are currently no clear guidelines regarding whether AS should be de-escalated after years without progression.
(Source: Dr. Kevin Shee, UCSF based on my MedPage Today story)
We wanted to know:
1) the upgrade outcomes over time for patients who like Howard are diagnosed with 3+3 prostate cancer initially but do not progress for multiple biopsies;
2) the rates of metastasis and death from prostate cancer in these patients on AS, and
3) factors associated with upgrade so we may better choose patients for de-escalation. We felt that we could use our well-established AS outcomes database to get some initial answers.
We identified 774 men who had at least 3 biopsies on AS with 3+3 (GG1) prostate cancer without progression of disease for 5 years, meaning that they never upgraded to 3+4 in the time on AS. We looked at their outcomes over time and to our surprise we found a surprisingly large amount of upgrade events.
Nearly 50% of patients upgraded to at least 3+4 (GG2) at 10 years, and almost 80% upgraded by 15 years. Although the rate of upgrade was high, management with AS was very effective, and only 1% of patients developed metastasis at 10 years and 2% at 15 years, with no patients dying of prostate cancer over the same duration of time.
We further identified increased age, body mass index (BMI), PSA density, and biopsy core positivity as significantly associated with upgrade from 3+3 on AS.
We conclude from these findings a few things. Because of the high rate of upgrade in this cohort without initial disease progression for 5 years, we support continuing AS for these patients, particularly in those with life expectancy >10 years. We also think that certain patients, for example those with low-core positivity and PSA density, can benefit from deintensification of AS, although the specific follow-up protocols for this deintensification wasn’t within the scope of this manuscript. Finally, we again show that AS is a safe and effective management strategy for 3+3 prostate cancer, and that rates of metastasis and death from prostate cancer are extremely low.
We want to thank Howard for lending patient insight into this clinical question, and for really being the main motivation behind this study. Dr. Carroll and I hope that this research opens the door to a thorough investigation into the appropriate deintensification protocol for stable AS patients, and for eventual inclusion in prostate cancer guidelines.
(Thanks Dr. Shee and Carroll. I will be discussing this study with my personal physician. I have some idea on what I will do—at least for the next two years.)
(AI rendition of DNA.)
Last chance to register for the ASPI DNA webinar on Saturday
Why All Men Diagnosed with Prostate Cancer Should Undergo Germline Genetic Testing—ASPI meeting
It’s time to spit for science and undergo germline genetic testing to see whether we carry mutations inherited from our parents that have a potential impact on the course of Active Surveillance for low-risk prostate cancer. Testing also can yield significant information for our closest relatives about mutations not only for prostate cancer but breast, colon and other major cancers.
Active Surveillance Patients International’s July webinar features a panel of experts to address this topic. The session will run from noon to 1:30 pm Eastern time on Saturday, July 26. Please register for the meeting here
The panel includes:
Neal Shore, MD, a urologic oncologist and Medical Director for the Carolina Urologic Research Center in Myrtle Beach, S.C,. and Channing Paller, MD, a medical oncologist at Sibley Memorial Hospital, an associate professor of oncology at the Johns Hopkins University School of Medicine and lead investigator of the Promise study of genetics and prostate cancer. Drs. Shore and Paller were co-authors of a recent article in ASCO Oncology Practice, calling for universal germline testing in prostate cancer patients.
Neil Perlman, M.D., Medical Director of Colon Cancer Alliance for Research and Education for Lynch Syndrome, will round out our panel. Not only is Dr. Perlman a Chicago-based internist, he also is a patient with Lynch syndrome and an advocate for patients with this hereditary disorder, which has significantly increased risk of cancer of the prostate, colon, uterus, and ovary. Dr. Perlman has been lobbying for changes in state laws to protect patients’ genetic rights and access to insurance.
There will be a Question and Answer session following remarks by our panel.
Please send questions in advance to: contactus@aspatients.org
New Research Study at NYU Langone Health for Hispanic Patients with Prostate Cancer
“Perspectives on Genetic Testing for Prostate Cancer”
Why is this study being done?
• To understand what Hispanic patients with prostate cancer think about genetic testing.
Who may take part in this study?
• Hispanic
• Have prostate cancer
• Age 18 years or older and live in the United States
What will participation in this study involve?
• Completing a questionnaire online
• Taking part in a virtual interview using WebEx or Zoom (online meeting platforms) lasting approximately 40 minutes
• Gift card for study participation
Participation is voluntary. For more information, please contact us:
• Nataliya Byrne: Nataliya.Byrne@nyulangone.org • 646-501-2681
• Tatiana Sanchez Nolasco: Tatiana.Sancheznolasco@nyulangone.org • 646-501-2550
• Mariana Rangel: Mariana.RangelCamacho@nyulangone.org • 646-501-2552
• Evangelia Pitsoulakis: Evangelia.Pitsoulakis@nyulangone.org • 929-573-0920
• Sukhleen Bedi: Sukhleen.Bedi@nyulangone.org • 646-501-3601
To confirm this study is valid:
• Contact the NYU Langone Health Institutional Review Board (IRB) at 212-263-4110
• Reference the study number (23-00993)
• Principal Investigator is Dr. Stacy Loeb, Professor in the Departments of Urology and Population Health at NYU Grossman School of Medicine



Maybe it's not about our particular cases. Maybe it's more important to contribute to data collection. My urologist told me I had a very slow growth type of cancer and if I died in the next fifteen years it wouldn't be because of the prostrate cancer. Bottom line is the doctors don't really know.
Out of the park Howard! I turn 72 in Nov and my next AS check-up is Sep. Should be interesting and will definitively fit within this discussion. I have become extremely averse to blind biopsies and want an imaging solution. That said, MRI remains, for lack of a better term, speculative. Based on everything I have seen, the µUltrasound has emerged as the 'right thing' in my opinion. Get a view at the same quality as MRI at a fraction of the cost, no Gd contrast agent, and if something suspicious is there the Uro can take a shot at it since it takes place at their practice. What we need is an AI that can dynamically assist the Uro as the images are captured, sort of like a radiologist looking over their shoulder during the procedure.