ASPI honors Michigan's Morgan for patient advocacy in 'Prefer-gate' scandal
Morgan speaks out on biparametric MRIs, exercise and more
By Howard Wolinsky
I recently visited my old stomping grounds at the University of Michigan in Ann Arbor (Go Blue!). Forty-plus years ago, I was a journalist-in-residence there in 1977-78. I studied the politics and economics of medicine, medical ethics, Nazi medicine, and more in the liberal arts school, the medical school, and the school of public health.
Our son Adam was born in Ann Arbor during the fellowship year. So I have a lot of connections to this wonderful town.
On behalf of Active Surveillance Patients International, on Aug. 2, I presented a patient advocacy award to Dr. Todd Morgan, chief of surgery at Michigan Medicine.
(Dr. Morgan shows off his ASPI patient advocacy award in his office.)
Morgan, Research Professor and Professor of Urology and Section Head of Urologic Oncology at the University of Michigan Medical School, played a key role in 2021 as a member of the prostate panel for the National Comprehensive Cancer Network, which writes guidelines on PCa
In September 2021, NCCN downgraded Active Surveillance from the “preferred” approach for men with low-risk cancer to being on par with surgery and radiation. Urologists consider the NCCN guidelines as their practice Bible. So this potentially was a major blow to Active Surveillance.
This was a shock to urologists and patients, and to researchers, who proved the benefit of AS over 25 years.
Dr. Matt Cooperberg, an AS advocate from the University of California, led a Twitterstorm to get NCCN to reverse itself in what is called “Prefer-gate” scandal. ASPI, AnCan, and ZERO Prostate Cancer all lobbied for a reversal.
Inside NCCN, Morgan stood up for patients and AS. In two months, NCCN reversed itself. Peace was restored in PCa-land.
ASPI honored both Cooperberg and Morgan for their advocacy. I presented Morgan’s award at MUSIC’s summer shindig for clinicians and staff, on a farm owned by faculty member, Dr. Casey Dauw in Dexter, Michigan, outside of Ann Arbor.
University of Michigan Urology got the word out on the award in X, formerly Twitter.
Watch the video of his talk and the award presentation:
https://aspatients.org/meeting/active-surveillance-past-present-future-with-dr-todd-morgan/
(Edited from Dr, Morgan’s talk:)
On the past, present and future of Active Surveillance
By Todd Morgan, MD
When the NCCN (National Comprehensive Cancer Network) guidelines changed in 2021, they put out edits. In edit version one, 2022, the words "Surveillance preferred" was struck through, and there were other modifications. What I can tell you about the process is basically nothing, because everything that happens in those NCCN meetings is totally confidential. Whether I spoke up or didn’t speak up is something I can’t discuss.
But yes, I thought that change was wrong and made no sense to me. I was thrilled—beyond thrilled—when it was reversed and our panel was able to correct it a couple of months later. To me, the problem at the time—and to some extent, still—is the overtreatment of low-risk prostate cancer, not undertreatment. This was the wrong move, and thankfully, it got corrected.
Now, here’s the present. Among the many algorithms in the NCCN guidelines, one nice thing is that they are very algorithmic. Of course, not every patient fits neatly into an algorithm, but there’s a basic structure for low-risk patients.
At this point, the top fork in the road says, "Active Surveillance preferred for most patients." Why just "most"? Well, there are times when patients with low-risk prostate cancer may desire or need treatment—those with very high-volume, low-risk disease, for example. NCCN rarely says treatment is not an option. Although for very low-risk prostate cancer, there isn’t a decision tree, just Active Surveillance. There’s more nuance in the broader low-risk population, but the rule says "preferred for most."
Where are we going? What are the problems?
I’m fortunate to be part of a huge study, the prostate cancer active surveillance study run by Dr. Dan Lin, also known as the Canary PASS study. This registry has been going on across 10 sites for over 15 years. University of Michigan is a site, and the recent publication was really the seminal one from that cohort, published last year in JAMA.
If we look at 2,000 plus participants—most with low-risk prostate cancer, some not—the data goes out to 12–13 years from starting surveillance. You see all-cause mortality—deaths from heart attacks, other cancers—going up over time.
Many of these patients are diagnosed at older ages; that’s why we don’t recommend treatment for everyone. Deaths from other causes are much more common than deaths from prostate cancer. Virtually nobody died from prostate cancer.
Metastasis does go up a bit over time. Of 2,000+ patients, about 21 developed metastasis over 12 years. So it’s not zero, it’s about 1%. This is the reality. It’s every man’s fear when being recommended surveillance for low-risk prostate cancer. They say, “99% sounds pretty good, but it’s not 100%.” We need to get closer to 100%.
So metastasis: 21 patients, prostate cancer deaths: three, and many more died of other causes.
Four thoughts on the future:
First, Active Surveillance rates will continue to increase and will include the intermediate-risk category. There’s a paper led by Randy Vince, currently at Case Western, who was one of our fellows at Michigan. MUSIC [Michigan Urologic Surgery Improvement Coalition] initiated a project, primarily led by Jim Montie [one of the founders of MUSIC and Morgan’s mentor who attended the award ceremonyon Zoom] and David Miller, in 2014–15 to address low and variable statewide surveillance rates.
Rates have risen; in low-risk patients, it’s now upwards of 85–90% managed initially by surveillance. SEER [ Surveillance, Epidemiology, and End Results program] rates initially matched MUSIC, but have not increased as rapidly. Other data suggest national surveillance rates are markedly rising, finally at 50–60% in low-risk disease. Even in Michigan, recent data shows rates ticking up in an S-pattern. We feel confident that surveillance is safe for the vast majority of low-risk, and even some intermediate-risk patients.
Second is the future of digital pathology and AI. When a biopsy is done or tissue removed, it’s put on a glass slide for the pathologist to view. Now those images are digitized and uploaded; at Michigan our pathologists, as of last fall, primarily review digital images instead of glass slides.
That means images can be subjected to AI analysis. The classic is a neural network that interprets the data, fed inputs, and outcomes. One platform, among several, uses both clinical data (age, PSA, grade, margins, T-stage) and image data from pathology to provide risk prediction. Image-based info adds tremendous predictive power.
Ultimately, I think there will be many companies doing this—it will be commoditized. Any tissue sample will soon go through these models. Pathologists will still be key, but risk prediction will get much more accurate, driven by these models. Artera AI and multimodal models perform exceptionally well, having been tested on vast numbers of patients, both prospectively and retrospectively. It’s clear that the image-based information, stacked with our usual prognosis tools, allows clear stratification of risk. We may not know exactly what the AI is seeing, but what matters is its accuracy.
Third is the adoption of biparametric or non-contrast MRI. This has become prominent in the last few months.
Many in the urological oncology community aren’t yet aware, but they will be—contrast likely isn't necessary for most prostate MRIs. Omitting contrast saves time, is less costly, avoids IV and potential reactions, and is more efficient. Contrast is helpful only in some instances, but turns out doesn’t add much.
AUA (American Urological Association) guidelines highlight multiparametric MR; what's the difference? The multi approach adds dynamic contrast-enhanced phase.
Dr. Ben Pocross at Michigan researched cost differences—contrast MRIs are about $500 more. But is it as good? A recent big trial, the PRIME trial, compared biparametric and multiparametric MRIs with biopsies interpreted accordingly.
Clinically significant cancer detection rates—Gleason 3+4 or above—were 29% for multiparametric, 28.8% for biparametric MRIs; only two or three patients overall showed a significant difference. We’ve converted the vast majority to biparametric MRI in Michigan just this past year, and our data is in line—it's just as good.
Finally, my last and perhaps most exciting comment: The most common patient question I get is, “Aside from your plan, doctor, what can I do?” Our answers have been generic—avoid processed food, exercise, get good sleep, minimize stress.
But there are high-quality studies on diet and stress interventions for prostate cancer surveillance. For example, the MEAL study led by Dr. Kelly Parsons in JAMA randomized patients to increased vegetable intake, did not impact progression. A negative study.
But the most exciting study this year is on colon cancer. Structured exercise—patients who had surgery for colon cancer, followed by chemotherapy, were split into a control group (generic advice) and an exercise group (three years of support from a physical activity consultant). The exercise group had far superior disease-free survival—fewer recurrences, more prolonged survival. These are major differences on Kaplan-Meier curves, usually seen with some "home run" drug, but here it was exercise. The most common regimen: four 45-minute brisk walks per week. Brisk, but not fancy—getting a little short of breath. That’s my recommendation to patients now: brisk walking, four times per week. Will it work for prostate cancer? We don’t know, but there's no harm in trying.
With that, thank you to ASPI, and thanks, Dr. Jim Montie for the great introduction. This means a lot. Our urologic oncology team at Michigan is amazing. My getting to be here is partly because Dr. Montie called me out of the blue when I was a fellow, said, “We’ve got a great team at Michigan—will you come take a look?” And tell you what, we really do—you’re looking at an amazing, phenomenal team, and frankly, they mean the world to me.
ASPI honors Dr. Todd Morgan for patient advocacy
By Howard Wolinsky
In September 2021, by deleting one word, the prostate cancer panel of the National Comprehensive Cancer Network (NCCN), published a new guideline that reversed 25 years of research demonstrating the value of Active Surveillance (AS), close monitoring in managing low-risk prostate cancer.
A single doctor at the panel meeting, Todd Morgan, MD, professor of urology and chief of the Division of Urologic Oncology at the University of Michigan, opposed the change that eliminated the word “preferred” for AS, putting the management approach on par with radical surgery and radiation therapy.
The incident, known as “Preferred Gate,” resulted in Matthew Cooperberg, MD, professor of urology at UCSF School of Medicine, rallying opponents to the changed guideline through a “Twitterstorm.”
Within three months, NCCN, the leading guideline-writing organization, reversed its guideline and restored AS as the preferred management approach for low-risk prostate cancer. Active Surveillance Patients International (ASPI) has presented its Special Award for Advocacy for 2025 to Morgan and Cooperberg.
(There is a separate report on Dr. Cooperberg.)
These two distinguished urologic oncologists not only have done outstanding research on AS, but they have also played important roles in restoring the status of Active Surveillance as the preferred approach to managing low-risk prostate cancer.
As a cofounder of ASPI and chairman of the awards committee, I presented an award to Morgan in Ann Arbor on Aug. 2
Jim Montie, MD, professor emeritus of urology at the University of Michigan, a pioneer in AS<, portrayed Morgan as a strong advocate for his patients and for AS.
“Having been in the room during NCCN Guideline deliberations, it is difficult to stand up against the flow of the discussion. Todd's commitment to the value of AS and a deep understanding of providers' reliance on guidelines in decision-making, gave him the courage to stay the course in support of AS recommendations,” he said,
Morgan said the dealings of NCCN are confidential so he can’t share details on what happened at its meeting that led to the demotion of AS.
He said the members of the prostate panel are all experts, but also independent thinkers: “It is okay when we have a guideline come out, and then for us to have our separate independent thoughts on the guideline. Of course, not everybody agrees with every statement that's in the guideline. It was acceptable for me to say, ‘Look, yeah, that's the guideline, but I don't agree with it.’ And I don't agree that active surveillance should have been de-emphasized. That was certainly my broad position at that time, again, not speaking directly to what happened inside the room.”
Once the guideline was released, Cooperberg launched a Twitterstorm--a campaign of tweets-- resulting in “outrage” among urologists.
Morgan said, “Social media served a real purpose, because it brought visibility to this change. Historically, NCCN releases a new guideline on its website, but people typically don't discover it until they decide to review the guideline again, which might be months later.
“And in this case, it really catalyzed the moment where some of the leaders in the field said, hold on. What the heck is this about? Why would we make this change? This isn't right and drew a lot of attention to it. And what it did is it put some pressure on the NCCN to re-evaluate it. And again, I can't speak to what was happening on the inside of the panel, but clearly it did force a re-evaluation that then happened within a pretty short period of time.”
Montie, founding co-director of the Michigan Urologic Surgery Improvement Collaborative (MUSIC), noted that Morgan has had 275 peer-reviewed publications, 50 of which are related to AS in prostate cancer.
Morgan has initiated two prospective clinical trials on the role of gene-expression classifier testing in patients with localized prostate cancer (G-MINOR and G-MAJOR), each involving hundreds of patients through MUSIC.
Morgan said: “One of the things I love about urologic oncology is, yes, we're surgeons. But we are clinicians and oncologists first. And it's not ‘we're a hammer, and the world is full of nails.’ If there's a patient in front of me, and the patient is at a difficult time in their life, and maybe their disease is not aggressive, but it's a big deal for them. Our job is to not be a one-size-fits-all.”
Previous winners of the ASPI Special Award were: 2024, Drs. Freddie Hamdy and Jenny Donovan, principal investigators of the ProtecT trial and the more than 1600 randomized patients in the study. ProtecT proved AS was as safe as a management technique as radical prostatectomy and radiation therapy.
In 2023, the MUSIC won for showing how the efforts of urologists in cooperation with a leading insurer, Blue Cross/Blue Shield of Michigan, can increase uptake of AS.
The uptake of AS in Michigan is more than 90%, comparable to that in Sweden and the United Kingdom. The national average in the United States is 60%.
Mark Lichty, cofounder of ASPI and its chairman, said “We have designed these awards not just to honor the recipients, but also to share the ASPI message of patient empowerment and the patient voice in the prostate cancer journey. The hands depict the importance of both the patient and doctor listening to one another.”
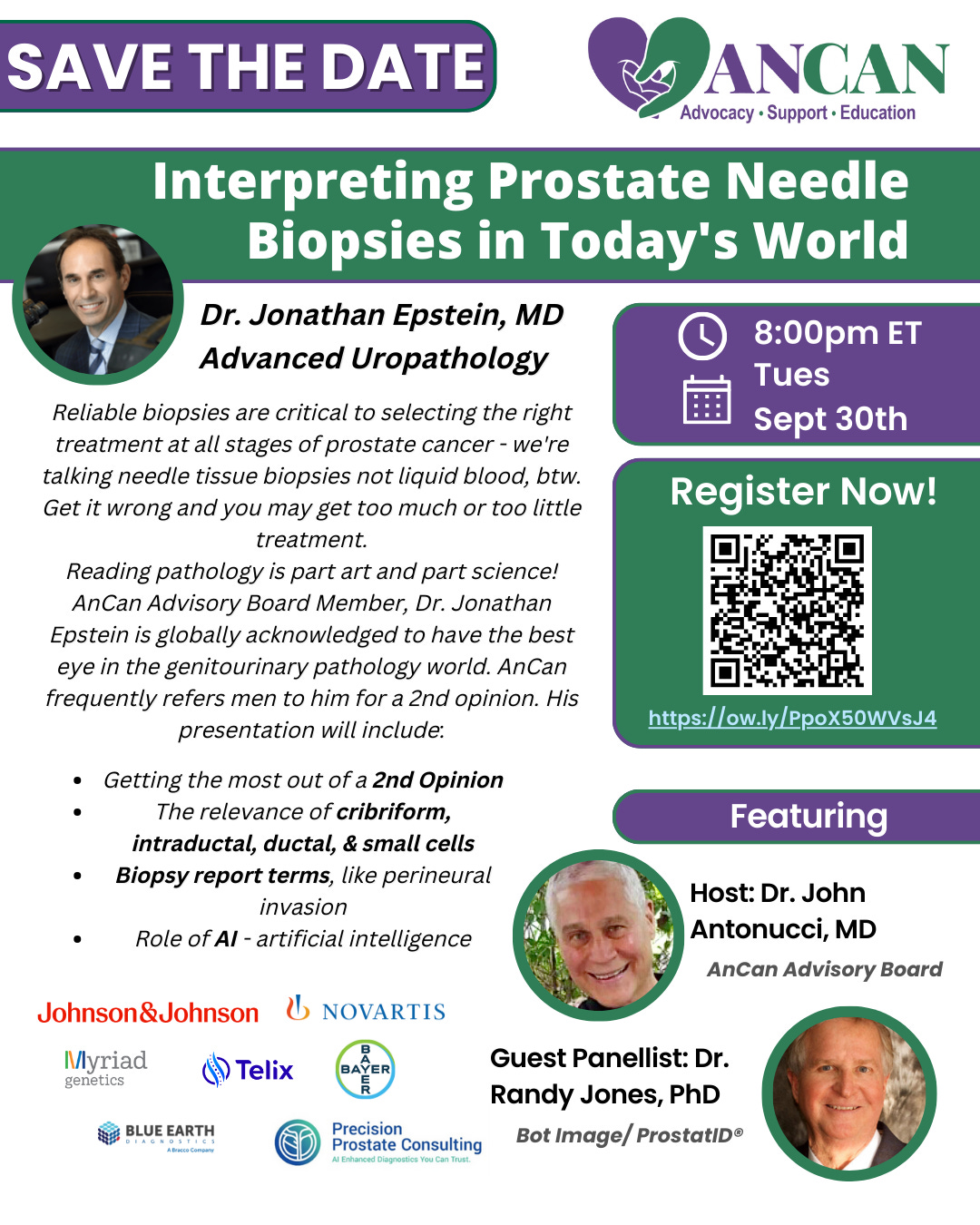
Register for Dr. Epstein: https://ow.ly/PpoX50WVsJ4
At AnCan on Sept. 17: MRI 2nd Opinions..... ProstatID solves the challenge
Getting second opinions essential in PCa care.
It's easy to find a medical 2nd opinion, and you can get your pathology reread by the best. But MRIs - that's been challenging.
Now there's an affordable AI-validated option that's proven very reliable* - ProstatID from Omaha-based Bot Image. Medicare covers ProstatID.
Join AnCan on Wed. Sep 17th at 6.30 pm Eastern in the AnCan Barniskis Room https://www.gotomeet.me/AnswerCancer Free & drop-in, precdeing AnCan’s weekly virtual support session for patients on Active Surveillance.
Founder and Developer of Bot Image, Randall Jones, PhD , MBA,explains the technology and its uses. Hosted by AnCan Advisory Board Member and prostate cancer peer, Cdr. Mike Crosby, who is chief commercial officer at Bot Image.
ProtatID is licensed to medical groups and also is available from Precision Prostate Consulting, in which Jones is a partner.
You can get a preview of Bot Image in The Active Surveillor:
Has the time come for AI and MRIs?
·
(Editor’s note: We’ve heard a lot about AI and pathology reports.
Up next At ASPI: What’s up with BPH
By Howard Wolinsky
Patients with low-risk prostate cancer are no strangers to BPH (benign prostatic hyperplasia), an enlarged prostate.
The percentage of men with low-risk prostate cancer who have (BPH) is not precisely stated in the medical literature. But autopsy and epidemiological data suggest that more than 20% of men with prostate cancer also have BPH, with some older studies showing this co-occurrence in up to 83% of prostate cancer cases overall.
Since BPH prevalence rises with age, and most low-risk prostate cancer patients are older, overlap is common. Many men diagnosed with low-risk prostate cancer are found through PSA testing, which BPH often also elevates.
BPH has been a focus of a lot research, such as water vapor ablation, which also is under study as a prostate cancer treatment.
(Dr. Brian Helfand)
Learn more at the next webinar by Active Surveillance Patients International, “BPH: What’s New, What’s Next,” featuring Brian Helfand, MD, PhD, who researches prostate cancer, AS, and BPH.
The program will be from noon to 12:30 p.m. Eastern on Saturday, September 27.
Register here.
In other news
Share how you found your prostate cancer specialist:
New Research Study at NYU Langone Health for Hispanic Patients with Prostate Cancer: Dr. Stacy Loeb and Colleagues are conducting a new study “Perspectives on Genetic Testing for Prostate Cancer” for Hispanic patients with prostate cancer. Participation involves an anonymous 40-minute virtual interview, in English or Spanish, to share perspectives about genetic testing. A $40 honorarium is provided for participation. For more information, please contact the study coordinator Tatiana Sanchez Nolasco (Tatiana.Sancheznolasco@nyulangone.org or 646-501-2550).






I was once in Ann Arbor at the Michigan university's library, 2009 along with our good friends from Waterford, MI. It's really a nice place!
So glad to see bi-parametric getting more press. In my attempt to avoid a(nother) MP-MRI with Gd, I foolishly thought a µUltrasound would fit the bill since it is 'non-inferior' to MRI. Well, the foolishness comes from thinking that an U/S scan is the 'same' as an MRI because of that pesky medical term 'Non-inferior'. It isn't at all and the major difference is geometric. With MRI, you are immobile and highly constrained during the scan (ask Howard, he loves this aspect of the scan 😉) which produces very detailed, high resolution images that are geometrically aligned and spatially accurate.
As a side note, getting gland volume from MRI is superior to U/S is superior (and it's ridiculous to even compare) to DRE. MRI is considered the 'gold standard' for volume measurement. Prostate volume is EXTREMELY critical to diagnosis and treatment, but I digress. With µU/S, you essentially have a probe that is 'all over the place' because it is in the hand of the clinician waving around up inside your...ahem. Yes, the wand can be stabilized, but still nothing like the milieu of an MRI.
If you have an MRI before the µU/S exam, the imagery can be fused and that is actually preferred over 'just a µU/S exam'. µU/S is also restricted by gland volume, ≥80cc causes issues because the wand can only get in there so far.
So, nobody does µU/S scans for the reasons presented. If you have a µU/S be prepared for needles because it is accompanied by a biopsy. I am very much anti-biopsy, period, but if I needed one I would do µU/S.