MRI shines a light on whether we need biopsies
Saying no to Torquemada the Tech. End the 'Prostalogic Inquisition.'
By Howard Wolinsky
Multiparametric Magnetic Resonance Imaging (MRI) is becoming a standard in determining whether we need biopsies.
It wasn’t always that way.
I was in the first group of patients in the U.S. who underwent MRIs--but not so much for determining whether we needed a biopsy. In fact, in 2011, I had a biopsy first and then an MRI. At the University of Chicago 12, that’s how it was done.
In the following decade, MRIs have become increasingly accepted in determining whether to do a biopsy and also are used in fusion biopsies to determine where to target the needles.
I wasn’t a big fan of MRI in 2010. The scan was a mess in my case. I experienced things you likely won’t.
There were two delays in the scan. First, someone forgot to order a rectal probe. Then, the previous patient in the suite DIED. Can you believe they told me that after I informed the tech and radiologist, I am claustrophobic?
Then, the tech took on the infamous role of Torquemada the Grand Inquisitor, who used torture to find out whether converso Jews (converts to Christianity) were still practicing Jewish traditions in secret.
I didn’t expect the Spanish Inquisition. Nobody expects the Spanish Inquisition, as the comedy troupe Monty Python warned in skits in 1971. But I really didn’t expect the Urologic Inquisition, either.
Torquemada the MRI Tech tortured me by threatening me when I started to panic as I was head-first in the tube with the machine constantly banging.
I asked for a break. “Are we going to do this or what?” she railed. She said she would pull the plug on the scan if I didn’t calm down. I white-knuckled my way through as the magnets banged loudly.
She wouldn’t tell me how far along I was in the scan. She was gruff and nasty. Probably a burnout who saw fear in the eye of patients and just made things worse. No compassion or humanity.
She also did a poor job of inserting hearing protection. The foam fell out. I ended up with tinnitus--a result of constant MRI banging that I can hear even as I write this.
I called and complained to the radiologists. My brother happens to be a doctorate audiologist. He called to check on my scan and diagnosed tinnitus.
I had called the radiology department, but the radiologists refused to speak to me directly. They answered questions through a non-radiologist staffer.
I got the silent treatment. They probably thought I wanted to sue. I wrote to the new medical center CEO. I wanted to address the issues.
The non-physician administrators of the radiology department--even ignored the ombudsman who took up my case.
Six months later—you know I am persistent if nothing else—they fell over themselves apologizing—no doubt orders from the hospital CEO. I didn’t care about an apology. I was satisfied with the promise that Torquemada would be retrained in reassuring panicky, claustrophobic patients.
(Be wary of insensitive techs and uncommunicative radiologists.)
I suspect this won’t happen to you. What can you do to protect yourself? See if you can go into the tube feet first and be sure your ears are protected.
It might help to listen to music. (The music system at UChicago had been busted for months.)
It experienced a perfect storm in the radiology suite on a cold winter day in Chicago. And can you believe it, my parka and shirt were missing when I returned to my dressing room. (A patient with dementia went shopping and liked my duds.)
I switched doctors and hospitals in 2016 and have had the only other prostate MRI in this 12-year journey. I went in feet first, and the tech kept me informed of how far along I was in the scanning process, which helped me sail through it.
As much as I dislike MRIs, I dislike biopsies even more. I’ve had six biopsies in 12 years--I haven’t had another since 2016 as a baseline with the new doctor, who recommended biopsies every two years rather than the annual ones initially recommended for me at the other urology office.
Subsequently, I had spoken to experts like Dr. Laurence Klotz, the “father” of active surveillance, who was doing biopsies every three or four years, (He and several other gurus told me to stop undergoing biopsies because my PSA was steady at about 4.5-5 and because my so-called low-risk Gleason 6 cancer was seen only in a single biopsy in 2010.)
Then, in 2018, I read an article in The New England Journal of Medicine that endorsed the concept of using MRIs to monitor prostate cancer and reducing the use of biopsies. This was an international team, which, ironically included my UChicago urologist, who did my complaint to the radiology department.
I shared this study with my new urologist. I told him that based on my experience in leading support groups for men with low-risk prostate cancer that men were fed up with all the biopsies. They feared risks for potentially deadly and disabling sepsis and other infections from transrectal--AKA transfecal--biopsies. Some doctors had high infection rates as the fecal matter was pushed into their patients’ otherwise sterile prostate glands.
I predicted to my urologist in 2018 that there would be a patient revolt unless urologists changed their practices STAT. The response from a doctor who most of us would consider a “mensch,” to use the Yiddish vernacular? “Tough,” he said. “The biopsy is the best tool I have. It’s the gold standard.” Oy, a blind biopsy was the best they could do?
Still, I have been amazed at my urologist’s transformation—at least in my care. I expected last year he would recommend a biopsy at worst or an MRI at best for me.
Since 2017, I have been ready to pack my bags and undergo a micro-ultrasound in place of an MRI available in St. Louis or Cleveland if my doctor recommended another MRI. (Micro-ultrasounds are not available in the Medical Mecca of Chicago. I can only guess at the reasons.)
To my surprise, my doctor recommended neither an MRI nor a biopsy.
He told me my PSA test (a special one known as the PHI test--Prostate Health Index) had been steady. He suggested that we continue monitoring my prostate with annual PHI tests and skip MRIs and biopsies unless my PSA started to trend up. (My PHI test this year fell 25%. Who knows why?)
I accepted this proposal. It may not be a good fit for anyone else. ask your doctor.
Monitoring by MRI is becoming the first step to avoiding unnecessary biopsies.
“Even though a biopsy is a minor, generally low-risk procedure, there are physical and psychological risks to any procedure,” said Dr. Benjamin Ristau, UConn Health’s surgical director of urologic oncology. “We want to minimize these risks as much as possible. MRI is one tool that allows us to do this.”
UConn has been a leader in active surveillance since its beginnings in the late 1990s. By chance, Connecticut had the nation’s only registry of prostate cancer patients. This helped urologist Peter Albertsen become one of the pioneers in AS. Mainstream urologists—the “grey eminences”—belittled him and the other early adopters of a non-surgical, non-radiological approach to Gleason 6 lesions.
Ristau recently contributed a commentary on prostate MRI for a special prostate cancer edition of the American Urological Association publication AUA News.
( Dr. Benjamin Ristau, UConn Health’s surgical director of urologic oncology. Photo by Tina Encarnacion)
Analyzing findings from several studies on MRI’s reliability in detecting prostate cancer, Ristau suggests that in many cases the MRI can tell doctors enough to guide an informed decision on performing — or confidently avoiding — a biopsy, in consultation with the patient.
There’s some interesting data here.
“Approximately 10% of clinically significant cancers are MRI invisible, so your urologist may continue to follow your PSA even if you have a normal MRI,” Ristau said. “This is especially true if you have prostate cancer risk factors such as family history of prostate cancer or African/Caribbean ancestry.”
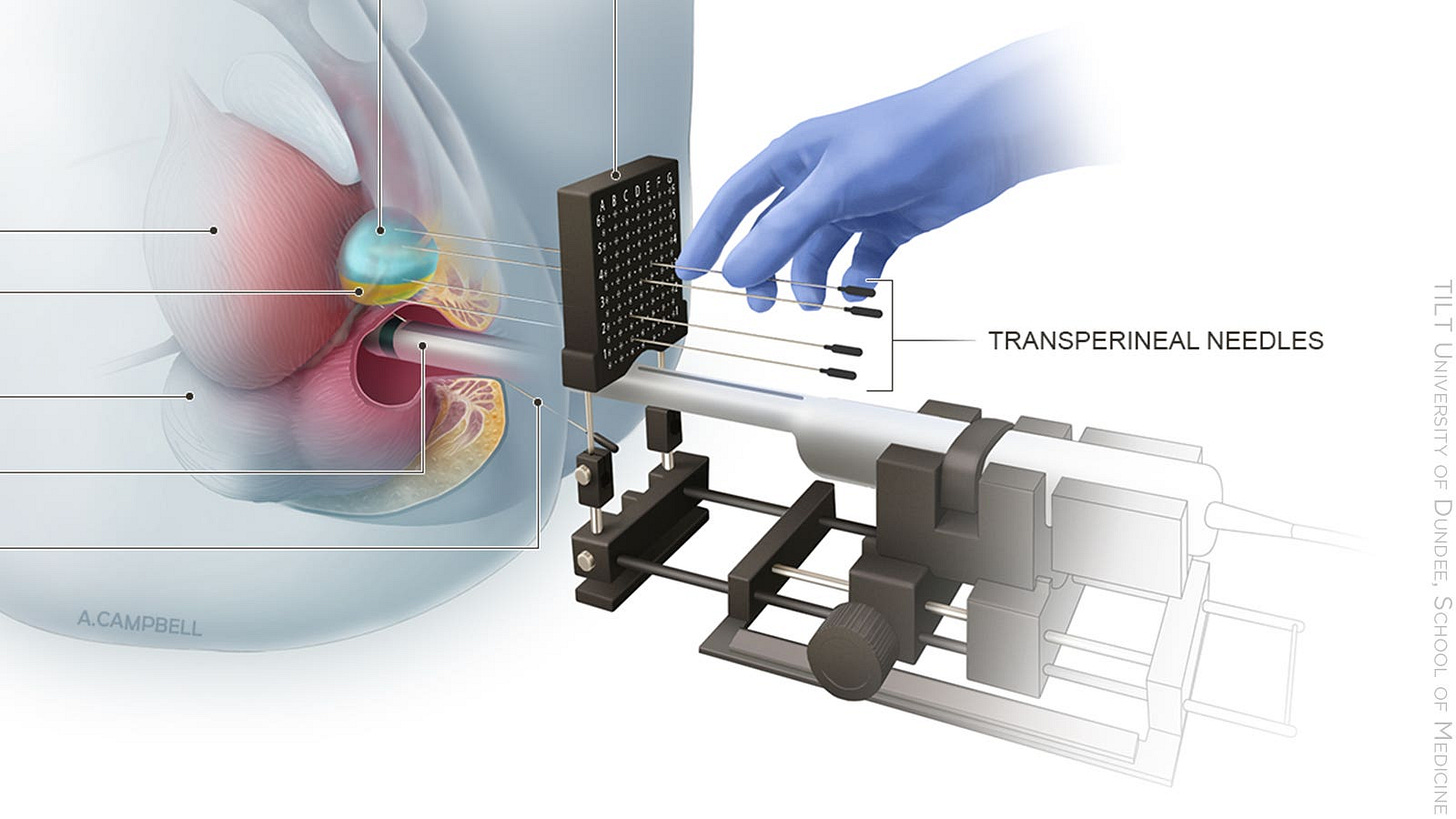
(Dr. Benjamin Ristau using ultrasound to guide him through a transperineal prostate biopsy at In the UConn Surgery Center. Photo by Kristin Wallace)
MRI results are graded on a scale of 1 to 5 known as the Prostate Imaging-Reporting and Data System, or PI-RADS. The higher the PI-RADS score, the greater the likelihood of prostate cancer. A score of 1 or 2 wouldn’t trigger a biopsy.
“PI-RADS 3 carries about a 12% risk of clinically significant cancers, PI-RADS 4 about 60%, and PI-RADS 5 about 85%,” Ristau said. “When we do not find a clinically significant cancer, we either find low-risk cancers (not clinically significant) or benign tissue (false positive). We routinely biopsy PI-RADS 4 and 5. Occasionally, we will biopsy a 3 if there are additional concerning risk factors, such as high PSA density, low percent free PSA, or family history.”
When a biopsy is necessary, UConn Health urologists perform a transperineal biopsy, a technique they say enables greater precision than the traditional approach and eliminates statistically significant risk of infection.
(Transperineal biopsy illustration from Medpagetoday.com.)
UConn Health urologists have been offering transperineal biopsies since 2019 and report zero associated infections. They also are participating in a multisite clinical trial led by Cornell University and funded by the Patient-Centered Outcomes Research Institute to compare the transperineal method to transrectal biopsy, which remains the standard of care in a majority of U.S. hospitals.
The American Urological Association will address the biopsy issue in 2023. In 2021, the European Association of Urologists threw its weight behind transperineal biopsies. Urologist Hendrik Van Poppel, policy chief for EAU, recently told me that in effect transrectal biopsies are considered “medical malpractice in Europe.”
UConn’s Ristau said, “The goal is to determine which technique is least obtrusive to patients.”
It’s about time, right? Say no to Torquemada. End the Prostalogic Inquisition.
Come to an Active Surveillance 101 webinar
By Howard Wolinsky
Dr. Laurence Klotz, the “father” of Active Surveillance, is featured in the second video in the series “Active Surveillance 101” which will be presented at the Active Surveillance Patients International (ASPI) meeting at 12 p.m. ET on Oct. 29.
Register here.
AS 101 is a series of conversations between actual patients and their partners/spouses and leading prostate cancer experts covering essential questions.
The goal of this series is to reach all AS candidates, including those who have not yet been diagnosed with prostate cancer but have rising PSAs (prostate-specific antigen) blood levels to provide them with an introduction to AS.
We—The Active Surveillor was one of the organizers—want to provide the tools to help these patients formulate questions when they go to their family doctors, urologists, or oncologists.
(Nancy and Larry White, spouse/patient meet with Dr. Klotz in AS 101 video)
AS 101 also is aimed at newly diagnosed patients on AS and established AS patients who want a refresher.
The premiere of part 1 of AS 101 has just aired at the monthly meeting of ASPI. To view.
The video features a patient and spouse, Larry and Nancy White, a real couple from New Mexico, meeting with family doctor Dr. Stephen Spann, dean of the University of Houston College of Medicine, on a consultation about rising PSA, treatment options, and a referral to a urologist. The prostate cancer “journey” often begins in the office of a primary care physician like Spann to discuss rising PSAs and then moves on to other specialists, such as urologists like Klotz.
The ASPI program includes the video and a question-and-answer period with patients.
In part 2, the Whites meet with Dr. Klotz, who explains early-stage, low-risk prostate cancer. Again, there will be a Q&A.
Earlier this year, ASPI honored Klotz, of the University of Toronto, as the winner of the first Gerald Chodak Active Surveillance Pioneer Award. The late Dr. Chodak was Klotz’s mentor and also was ASPI’s first medical advisor.
In the new video, Larry White, a real prostate cancer patient and himself a physician, and his wife Nancy, who has been an AS advocate, interact with Klotz as in a simulation of a real patient-partner-physician visit.
AS 101 was created under the banner of the Active Surveillance Coalition, whose members include ASPI, AnCan’s Virtual Support Group for Active Surveillance, Prostate Cancer Support Canada, Prostate Cancer Research Institute and The Active Surveillor newsletter.
For more background on AS 101, go to the blog for the Society for Participatory Medicine.
A shout out from MUSIC, America’s leader in active surveillance with 91% uptake vs. 60% nationally. Saving prostates every day.
When I started the newsletter in January, I promised I would not charge for subscriptions to TheActiveSurveillor.com But some readers volunteered to help me cover overhead expenses for transcription, stepped up internet service, and so on. The newsletter remains free. But your paid subscriptions are appreciated.