New debate for transperineal biopsies: ¿Despierto o dormido? Awake or asleep?
Not ¿Quien es mas macho?
By Howard Wolinsky
Remember when Saturday Night Live was reliably funny? Or somewhat funny.
They had an ongoing skit, featuring Bill Murray, with the game show, "¿Quien es mas macho?" Who is the manliest?
Well, at a support group I attend for patients on Active Surveillance for low-risk prostate cancer, we have an ongoing mock debate over transperineal biopsies.
We agree on the benefits of transperineal biopsies in avoiding the risks of sepsis and other infections from transrectal biopsies. (Rarely, patients can die from transrectal biopsies so transperineal procedures seem a safer bet—if you can find them.)
But we josh each other over whether to undergo the transperineal procedure by being knocked out with anesthesia to avoid pain from poking and prodding during a transperineal procedure, or to put up with a bit of momentary pain to avoid general anesthesia while receiving local anesthesia only.
Hence, we ask the new question regarding general anesthesia or no general anesthesia: "¿Quien es mas macho?"
It could be a game show for patients undergoing transperineal biopsies.
There is more to this than jousting over our manliness.
First, some background.
With transperineal biopsies, patients essentially can avoid sepsis and other infections as well as avoid powerful IV antibiotics, which contribute to the emergence of antibiotic-resistance superbugs and the declining effectiveness of antibiotics.
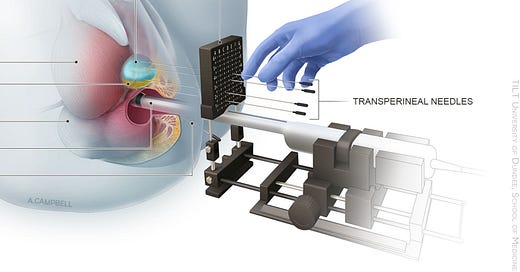
Transperineal biopsies, passing through the taint area, between the anus and the testicles, avoid these issues and also make it easier for urologists to sample hard-to-reach places in the prostate where cancer can lurk. Transperineal procedures easily reach the apex and anterior areas of the prostate, which often are missed in transrectal biopsies unless the urologist takes care.
Some urologists maintain that with proper attention they can use the popular transrectal biopsy--also referred to as the “transfecal” biopsy--to avoid most infections and effectively reach those out-of-the-way places in the prostate.
I have a cousin who is a urologist at a famous hospital. She rejects transperineal and doesn’t believe transrectal is a problem.
I asked her to sign my petition calling for a phase-out of transrectal. (Why don’t you sign?)
My cousin declined and said: “I haven’t done a recent side-by-side comparison of transperineal vs transrectal prostate biopsy risks but I don’t think that transperineal is overall better nor feasible on a large scale.” If she hasn’t checked, how does she know? There is some arrogance here and disregard for patient safety. But she is a nice person. I asked her urologist dad about signing. He said: “No.”
I think, unfortunately, they are typical of urologists in the U.S.
But American patients have begun voting with their feet and their prostates to go to urologists offering transperineal procedures. Danny Vesprini, MD, a radiation oncologist and head of Active Surveillance at Sunnybrook Health Sciences Centre at the University of Toronto, said, told me: Patients should tell their transperineal-resistant doctors: “I'm going to take my business elsewhere … I mean, it's a business.”
Transrectal biopsies have nearly gone extinct in Norway, Australia and the United Kingdom. Not here in the good ole U.S.A.
A guideline committee of the American Urological Urological Association will address these issues in 2023. U.S. urologists lag behind their colleagues from the European Association of Urologists, which in 2021 endorsed transperineal procedures over transrectal ones as being the preferred technique. Some insurance schemes, such as in Australia, pay urologists who offer transperineal procedures considerably higher fees.
Though American doctors are debating the matter, I suspect most patients, who hear the facts, would prefer transperineal biopsies over transrectal biopsies.
This leads to the next question about transperineal being debated amongst patients: ¿Despierto o dormido? Awake or asleep?
Some men fear the pain and would rather be knocked out and face the minor risks of general anesthesia or other techniques. Others tell me the pain from a transperineal biopsy is tolerable.
(Matthew Allaway, MD)
Matthew Allaway, DO, inventor of the PrecisionPoint method for doing transperineal procedures, said his system was designed with the idea that the patient would only undergo local anesthesia and would remain awake in an in-office procedure.
He said most of these procedures are done that way.
Grin and bear the pain, momentarily, if you can. Not all men can.
Historically, a transperineal route originally was used for prostate biopsies. I’m told men experienced a lot of pain and were put under in the OR. I suspect memories of this technique have lingered among some TP-averse urologists.
The biopsy gun changed everything in the late 1980s. Transrectals became the go-to procedure. Biologists had a zip gun to extract cores or samples. They even used to do them without local anesthesia.
It looks like a weapon that Ming the Merciless’ guards might flourish.
(Ming on right.)
Now the pendulum is swinging back to transperineal because of availability of new techniques and growing concern about sepsis.
Many patients are opting for general anesthesia or sedation in a hospital OR or surgicenter. There’s patient preference because of fear over the potential pain. There’s also doctor preference to go to the OR as they are gaining experience with TP.
Also, I know urologists who are strong advocates of TP with GA (general anesthesia) because of their perceptions of patient pain--though they've never undergone a biopsy themselves. It makes their job easier to knock out the patient and avoid squirming. It also helps with the workflow and saves time.
British urologist Rick Popert, MD, a leader in the TRexit (transrectal exit) movement to end transfecal procedures, told me: “The need for GA and antibiotics is dependent on the type of TP biopsy being offered to patients and as … the initiative started in the private sector rather than the public, and GA has been the norm, however with LA (local anesthesia) TP biopsy techniques being increasingly adopted practice is changing.
“In the UK we have been doing TP biopsies since 2006 and between 2006 & 2010, they accounted for no more than 5% of all prostate biopsies. Between 2010 & 2019, we saw a progressive increase in TP biopsies, accelerated by the introduction of pre-biopsy MRI, identifying anterior disease, so we could select better the type of biopsy. These were all grid-based mapping biopsies and almost all done under GA. The National Prostate Cancer Audit showed that these biopsies were associated with 1% risk of infection and associated with twice the risk of urinary retention.
“By 2019 TP biopsies accounted for 30% of all biopsies but with introduction of LA TP biopsy techniques and the impact of the pandemic in the UK, as of April 2021 the ratio has completely switched and TP biopsies accounted for 65% of all biopsies.
“It is a truism that it takes 10 years to become an overnight success. This has all been achieved within 3 years.”
(Richard Szabo, MD)
Richard Szabo, MD, a urologist at the University of California, Irvine, is a leading researcher on transrectal vs. transperineal. He thinks financial issues may be driving the move to the surgical suite, too.
He said, “I believe the main reason urologists choose the OR is to get the facility fee for the surgicenter, with which they usually share profits. It is certainly easier and faster to go to a transperineal prostate biopsy on patients who have undergone general anesthesia or intravenous sedation because it speeds up the local anesthesia instillation, or avoids it altogether, which saves time.”
On the antibiotic issue, he said: “Those who use antibiotics might not be ready to try without antibiotics and might worry about liability. However, there are adequate numbers of research papers out there to argue against using prophylactic antibiotics for transperineal biopsy; it's just a new direction for now.”
Allaway said, “We are encouraging patients to have their TP biopsies done under LA. This is a value proposition for the system since each level of anesthesia brings the cost up. However, my opinion of the data is that 10% of patients are not well suited for LA. I feel that patients should not be forced to have the biopsy under LA. If I was having a biopsy, I would absolutely do this under LA.”
I may be done with biopsies, my urologist told me, unless my PSA (prostate-specific antigen) levels increase. But if I have another biopsy, I’d choose a transperineal approach in the urology office.
(My personal urologist finally has trained with Allaway’s Perinealogic system.)
My feeling is why should I undergo general anesthesia if I don’t need it? Likewise, why have the antibiotics when the taint can be scrubbed and you can avoid infections?
Bottom line: I wouldn’t fault any patient who opted for a transperineal procedure with general anesthesia if it makes them more comfortable and gets the job done. You gotta do what makes you comfortable.
Awake or asleep, if you need a biopsy, go for a transperineal if you can. But if a transperineal is not available, and they can be hard to get, by all means, consider a transrectal. In general, urologists need to be more judicious about the use of these potentially infectious procedures.
(Side note: I think the choice to avoid antibiotics is a harder sell for urologists, who can use potent antibiotics like candy and provides them a sense of security.
However, research supports the idea of not using powerful antibiotics on these patients. Szabo lists the following:
Kohl, T., Sigle, A., Kuru, T. et al. Comprehensive analysis of complications after transperineal prostate biopsy without antibiotic prophylaxis: results of a multicenter trial with 30 days’ follow-up.Prostate Cancer Prostatic Dis (2021). https://doi.org/10.1038/s41391-021-00423-3
Islam, M., Da Silva, R.D., Quach, A. et al. Are outpatient transperineal prostate biopsies without antibiotic prophylaxis equivalent to standard transrectal biopsies for patient safety and cancer detection rates? A retrospective cohort study in 222 patients. Patient Saf Surg 15, 28 (2021). https://doi.org/10.1186/s13037-021-00303-8
Giacomo M. Pirola, Marilena Gubbiotti, Emanuele Rubilotta,et al. Is antibiotic prophylaxis still mandatory for transperineal prostate biopsy? Results of a comparative study,
Prostate International, 2021,https://doi.org/10.1016/j.prnil.2021.1 In Press
Take the transperineal quiz—awake or asleep? https://docs.google.com/forms/d/1VQZEa47XmiQygeU1mewBBaLIv9nkfAujjnYJknpWZlI/edit
Jeff Coleman tells all
(Exclusive interview. Jeffery Coleman, 62, an active humorist and retiree from Eldersberg, Maryland, who has a high-volume Gleason 6 diagnosis, tells TheActiveSurveillor.com why he opted for the OR when he had his second transperineal procedure at Johns Hopkins. He had only local anesthesia for his first transperineal biopsy.)
(Jeffery Coleman)
TheActiveSurveillor: Did you undergo transperineal under general anesthesia?
Jeffery Coleman: For clarification, I was not administered general anesthesia, meaning I controlled my own breathing. I was given MAC (Managed Anesthesia Care), which is also referred to as twilight anesthesia. This is the exact same type of anesthesia used during a colonoscopy. I chose anesthesia because I was unable to tolerate the discomfort (a polite word for PAIN!) of the ultrasound rectal probe.
--Did you have a choice?
The hospital does offer the choice but I was unaware that it was an option until after my second biopsy failed because I could not tolerate the discomfort (PAIN!) of the rectal probe. With all respect to the doctor though, he thought there would be no issue since my first biopsy was without anesthesia (the first was a different doctor who never mentioned using anesthesia). How I got through that one I don’t know. I do remember the doctor telling me to try and stay still, easy for him to say.
--What happened.
As mentioned, the first biopsy (September 2020) used no anesthesia; the second one (May 2022) did.
--Was that done in an OR?
Second biopsy while under anesthesia was done in an OR.
--Do you fear the pain of a transperineal more than the risks of anesthesia?
I had no “fear” of pain with the biopsy (needles). What I had was the knowledge that I could not tolerate the discomfort (I mean PAIN!) of the rectal probe. I really had no concerns with the anesthesia knowing it was MAC. I had had MAC twice before for colonoscopies and never had any issues with it.
--Were you even given a chance to have an office procedure?
Johns Hopkins does all of its biopsies in a surgical center. In a “standard” surgical room if no anesthesia, in an OR with anesthesia.
--Do you have concern about general anesthesia?
I have never had general anesthesia and probably will have some concerns with it were I ever to need it.
--What will you do the next time? If there is a next time?
The next time will be a no brainer (which is great for a guy like me with no brain, or the scarecrow from the Wizard of Oz)…..I will use anesthesia again!
--Any advice for men?
My advice for men is do not get prostate cancer (oh yes, and eat all of your vegetables). Unfortunately you cannot control getting PCa. If you need a biopsy, ask your doctor about the possibility of using anesthesia. My perspective is the less squirming around you are doing during the procedure, the easier it is for the doctor to hit the right spots while getting your samples. I have seen the length of those needles. One false move and he might be getting a sample from your spleen!
--Who is more macho? The guys without anesthesia? Or is it a tie?
This is easy, it’s the guys with anesthesia. If you are really macho, you don’t need to prove anything to anybody! Now if you’ll excuse me, I have to go bake some cookies.
Don’t miss the ASPI webinar, “Eat to Beat Prostate Disease,” on July 30 at 12-1:30 PM Eastern, featuring William Li, MD.
Free Registration: www.aspatients.org or go direct to: https://bit.ly/3t5lFLx
Free prostate-healthy recipes for all registrants.
Join Dr. Channing Paller, associate professor of Oncology and Urology at Johns Hopkins University, Sidney Kimmel Comprehensive Cancer Center, and Rob Finch, Director of Urology Medical Affairs at Myriad Genetics as they discuss the impact of genetic factors in prostate cancer and the PROMISE study.
Genetics, the PROMISE Study, and Prostate Cancer: a Town Hall Webinar
July 20, 6:00 p.m. - 7:00 p.m. Eastern Time
Meet the Speakers:
Dr. Channing Paller is associate professor of Oncology and Urology at Johns Hopkins University, Sidney Kimmel Comprehensive Cancer Center, and associate director for Oncology of the Johns Hopkins Clinical Research Network. She is a clinician scientist focused on translating basic scientific findings into treatments that will improve clinical outcomes and reduce toxicities for men with prostate cancer. Dr. Paller is a lead investigator of the PROMISE registry and, as an expert in clinical trial design, she leads multiple clinical trials of innovative new treatments and treatment combinations employing germline and somatic biomarkers. She earned her M.D. at Harvard Medical School and completed her medical residency and fellowship in Medical Oncology at Johns Hopkins.
-
Rob Finch is a Certified Genetic Counselor. He graduated with a Master’s Degree in Human Genetics from the University of Pittsburgh in May 2001. Rob worked at Memorial Sloan-Kettering Cancer Center from May 2001 to September 2003, where he led the Hereditary Colorectal Cancer Registry, as well as provided risk assessment and genetic testing to patients through the Clinical Genetics Service. In September 2003, Rob joined the Myriad Genetics Team, where he has served as a Regional Medical Specialist and Institutional Account Executive for the Oncology Division and currently serves as a Director of Urology Medical Affairs. Rob works to educate and provide clinical support to healthcare providers who treat prostate cancer for Myriad’s BRACAnalysis CDx®, MyRisk™ Hereditary Cancer Test, and Prolaris.
The Active Surveillor is a reader-supported publication. To receive new posts and support my work, consider becoming a free or paid subscriber.
Join a ZERO webinar, Prostate Cancer and the Unique Needs of the LGBTQIA+ Community featuring Anne Katz PhD, RN, FAAN, of CancerCare Manitoba, Winnipeg.
Register here:
https://us06web.zoom.us/webinar/register/WN_eUvLX0yNSAmRe5b-ST7zeg.









No mas, no mas por favor!
The ultrasound-guided prostate biopsy whether trans-rectal or trans-perineal and whether asleep or not, is an embarrassingly unscientific test. The 12-core test samples blindly and randomly about 0.1 percent of the prostate - when you add up the volumes of those 12 cores and measure it against the volume of your prostate. That leaves one totally ignorant of what is going on in the 99.9 percent rest of the prostate. A horrible sampling error rate. How ludicrous is that? If there is a benefit to the perineal route for the biopsy it's the fact that there are fewer septic (including deaths) and bleeding complications. All in all, the perineal biopsy is like putting lipstick on a pig - the ultrasound-guided biopsy (whether trans-rectal or perineal and whether asleep or not) is still a pig. This so-called test needs to be thrown out. The best way to detect potentially lethal high-grade disease (and ignore bogus disease) is with an MRI-guided biopsy by an expert - and then get a second opinion on the biopsy results.
An update on my own experience: My Trans-Perineal was done under general anesthesia; as it was a "Fusion" biopsy. This to make sure to accurately sample the area found on the annual MRI. I.E. no moving around and disturbing the process by the patient (me).
Additional data-point: Aetna Medicare Advantage plan still calls it "experimental" so the urologist fee was not covered. But, the rest of the hospital/anesthesiologist/etc. was covered.
Me thinks, another case of urologists (the ones at the insurance company) covering the general business practices of the majority of their fellow practicing urologists.
---I'm still glad I opted for Trans-Perineal. Got good data and no infection. A completely different experience from the TR biopsy.