WebMD tackles AS in older men
Our columnist Dr. Westphalen gives us the scoop on hip replacements, MRIs and AS
By Howard Wolinsky
Come this December, I will have been on Active Surveillance (AS) for low-risk prostate cancer for 13 years. I call it my “pros mitzvah.”
A local urologist—the “Notorious Dr. RP”— was trying to persuade me I needed a radical prostatectomy or radical radiotherapy yesterday. Back then, 94% of guys opted for treatment. Of course, only 6% went on AS in 2010.
But I lucked out because a friend at the University of Chicago told me they had an AS program there. Dr. Scott Eggener, an AS researcher, told me I was the “poster boy for AS,” the rest is low-risk prostate cancer history. It changed my life.
A handful of us looked at the research, such as that by Dr. Laurence Klotz from UToronto, that showed there was another way—AS—with close monitoring of a cancer that was unlikely to kill us. It was not a popular way to go in 2010.
But research has mounted, a new generation of urologists accepted that surgery is not the only way to go, support groups for AS have grown up, and an AS Army has risen up as patients see the advantages of avoiding what we politely call “quality of life issues” with aggressive treatment. QoL means treatment can put you at risk for urinary and fecal incontinence and erectile dysfunction.
In December 2021, 60% of U.S. men with low-risk cancer ride the AS train. AS has been an overnight success that only took 30 years. Not as good, as the 90% of low-risk patients on AS in the state of Michigan and the countries of Sweden and the United Kingdom, but still an improvement.
Now, many of us are thinking that AS has served us well as we hit our late 70s and 80s. And some are asking whether we should keep chugging along on the AS train?
Or should we dial it back and stop with MRIs and biopsies—as I have I have. I’ve only been watched with a type of PSA blood test since 2017, but I am ready for MRIs or biopsies if my PSA spikes. I call my strategy “passive-aggressive surveillance.”
Or maybe we should get off the train, not look back, and just live our lives?
Journalist Robert Fulton published a great article in WebMDcovering AS in older men interviewing my AS fellow travelers Allan Greenberg and Ira Kaget and experts Drs. Klotz, Dr. Kevin Ginsburg, of the Michigan Urologic Surgery Improvement Coalition (MUSIC), and Yale’s Dr. Michael Leapman, a columnist for TheActiveSurveillor.com.
Greenberg, a retired college prof, 83, told WebMD “At my age, treatment is the last thing I would consider … Even if it has seemed that things were getting worse, I'm not sure I would undergo any treatment at this point.”
WebMD asks: So if treatment is off the table, why even bother with surveillance?
“There's a wealth of literature showing that grade group 1 prostate cancer, in particular, is very, very different from other types of cancer,” said Kevin Ginsburg, MD, an assistant professor of urology at Wayne State University School of Medicine in Detroit. “As a consequence of that, the harms of treatment often very frequently outweigh the benefits."
Ginsburg, who is also the prostate program co-director at the Michigan Urological Surgery Improvement Collaborative, says the drawbacks of active surveillance -- the cancer spreading and killing the patient -- are low. A study from Johns Hopkins looking at a group of more than 1,800 men found that “the risk of cancer death or metastasis was less than 1% over long-term follow-up.”
Greenberg has often talked to me about quitting AS. Then, I know guys in their 80s who want to stay on AS until their 90s.
Take Kaget, a moderator with the Prostate Forum of Orange County.
He was diagnosed with low-risk prostate cancer in March 2009 at the age of 66. After the initial shock, Kaget, now 80, a retired marketing executive, researched the topic and spoke with experts. With a Gleason score of 3+3, he opted for active surveillance. He gets an MRI-informed targeted biopsy every 2 years and frequent PSA tests.
He observed his pros mitzvah last year and is looking forward to his pros-quinceañera next year. He plans to stay the course with AS, a genuine surveillance lifer.
“I plan to continue with this, continue monitoring, and I'm very intent on managing my case,” Kaget told WebMD. “The goal is to die with it instead of because of it.”
Readers have asked whether I have decided to stay on AS or to hop off the AS train. I have some time to decide.
I am still collecting your opinions. About 140 have responded but we can do better.
Please let me know what you think: https://forms.gle/oFvfH3rPdgJmEbiQ7 I’ll close the survey on Nov. 15 and will share the information soon thereafter,
If you are 75 or above, I’d especially like to know what your AS constitutes now, as your options for aggressive treatment like surgery decline, or how you’ve managed your care.
Check out my story in MedPage Today about what urologists think about staying on or leaving AS after age 75 and the need for guidelines: https://www.medpagetoday.com/special-reports/apatientsjourney/106873
Dilemma at 76: Stay onboard the Active Surveillance Express? Or hop off the train?
By Howard Wolinsky I’ve been a steadfast advocate of Active Surveillance (AS) since I was diagnosed with very low-risk prostate cancer in December 2010 and got on the AS train. And I still asupport AS for about half the 280,000 men a year diagnosed with prostate cancer.
Dr. Westphalen steps up to the plate on MRIs and hip replacements
By Howard Wolinsky
TheActiveSurveillor.com continues this week to roll out its series of Q&As with the experts. This week, Dr. Antonio Westphalen, a top radiologist specializing in theprostate at UWashington (Go Huskies or Malamutes), launches “The Radiology Report,” where he answers questions from readers on Active Surveillance.
You are invited to send questions to mailto:pros8canswers@gmail.com
Our leadoff hitter last week was Dr. Michael Leapman, a urologic oncologist from Yale (Go Bulldogs). Next week, Dr. Anne Katz, an author and certified sexuality counselor and Clinical Nurse Specialist at CancerCare Manitoba in Winnipeg, Canada, launches “Sexuality and Surveillance” followed by Ming Zhou, the pathology guru from Tufts Medical Center (Go Jumbos) with “The Pathology Report,” and, our newest addition, power hitter Dr. Stacy Loeb, of NYU (Go Bobcats), on “Lifestyle & Surveillance.”
Keep the questions short and sweet. They should be of general interest. Sign with your real name, or just initials, tell me where you live, how long you‘ve been on AS, how it’s going for for you. Share a whimsical signature if you’re so inclined.
Question: We have heard from numerous experts that having an MRI in the beginning, and "as needed" thereafter, is a necessary part of the AS monitoring protocol.
We have also heard that radiologists' readings and assignment of a PI-RADS score is, at best, subject to a varying degree of interpretation and accuracy based primarily on the degree of the radiologists' PI-RADS training and reading experience.
What we have not heard from the experts is to what degree having one or two metal hips make MRIs even more problematic and subjective in obtaining an accurate PI-RADS score due to artifact distortion. It would be nice to know if the experts can say that initial and subsequent MRIs are going to be subject to a fairly high degree of inaccuracy for the many of us for the many of us who have metal hip replacements. Question: We have heard from numerous experts that having an MRI in the beginning, and "as needed" thereafter, is a necessary part of the AS monitoring protocol.
We have also heard that radiologists' readings and assignment of a PI-RADS score is, at best, subject to a varying degree of interpretation and accuracy based primarily on the degree of the radiologists' PI-RADS training and reading experience.
We have heard from numerous experts that having an MRI in the beginning, and "as needed" thereafter, is a necessary part of the AS monitoring protocol.
We have also heard that radiologists' readings and assignment of a PI-RADS score is, at best, subject to a varying degree of interpretation and accuracy based primarily on the degree of the radiologists' PI-RADS training and reading experience.
Hip Dude from Maine Woods
What we have not heard from the experts is to what degree having one or two metal hips makes MRIs even more problematic and subjective in obtaining an accurate PI-RADS score due to artifact distortion. It would be nice to know if Dr. Westphalen can say initial and subsequent MRIs are going to be subject to a fairly high degree of inaccuracy for the many of us for the many of us who have metal hip replacements.
Dr. Antonio Westphalen: As the reader mentioned, the presence of hip replacements in a patient can reduce the quality of prostate images obtained through MRI scans. This happens because the metallic composition of the prostheses disrupts the magnetic field, which is essential for generating good images. Consequently, the diagnostic accuracy of such MRI scans can be compromised.
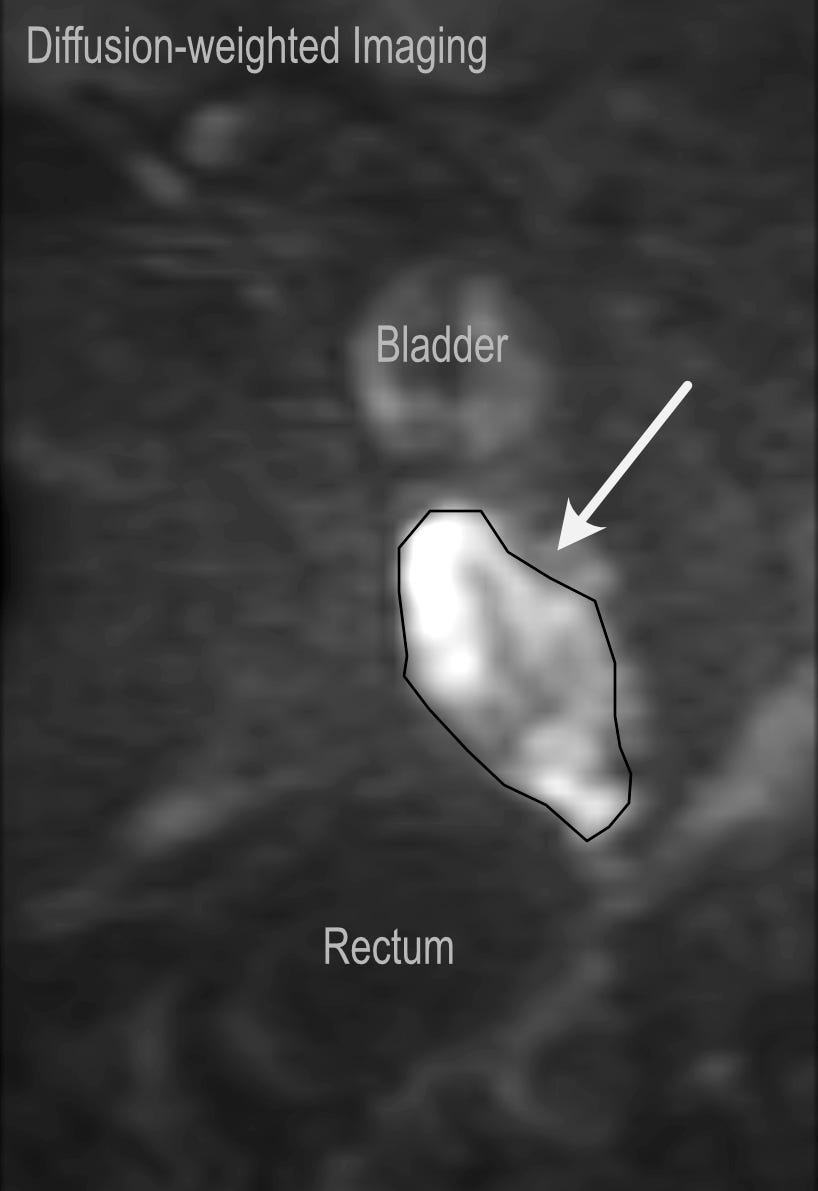
The degree of distortion encountered varies across different imaging sequences. The sequence that is most susceptible to distortion is the "diffusion-weighted imaging" (DWI), particularly critical for assessing abnormalities in the peripheral zone of the prostate. Conversely, for lesions found in the transition zone, the DWI assumes a secondary role in determining the PI-RADS score. The other two sequences, “T2-weighted images (T2)" and "dynamic contrast-enhanced images (DCE)," while also impacted by the presence of hip replacements, generally retain enough quality to be utilized for interpretation.
In situations where distortion in the DWI sequence is substantial, the recommended course of action is to repeat the DWI scan, if the source of the distortion can be resolved. However, this option is not viable for patients with hip replacements. In such cases, interpretation is based on the T2 and DCE sequences, particularly the former. DCE is only utilized to further characterize lesions that are assigned a PI-RADS score of 3 based on T2 findings.
(T2, little to no distortion. Courtesy: Antontonio Westphalen, MD.)
(DWI, distorted. Courtesy: Antonio Westphalen, MD.)
(Dr. Westphalen notes re images: “Same patient, same MRI. It illustrates how much a DWI can be affected by the hip prosthesis, while the T2 has not been impacted.)
The diagnostic accuracy of PI-RADS scores assigned without the inclusion of DWI has not been definitively established. Yet, based on research done prior to the creation of PI-RADS, it should be assumed to be lower than the accuracy of a PI-RADS score obtained with a complete study. Anecdotally, my observations suggest that radiologists may adjust their diagnostic threshold, potentially identifying more lesions than they would under normal circumstances. In practical terms, given that MRI scans are often performed with the primary intent of identifying target lesions for biopsy, reliance on T2 and DCE alone might result in an increased number of recommended biopsies.
Finally, it is crucial to emphasize that the distortion encountered in the DWI sequence does not invariably impact the precise location of a lesion within the prostate. In such instances, it remains feasible to assign a PI-RADS score following standard procedures.
Humorous update
By Howard Wolinsky
Remember the prostate humor contest? Several readers have reminded me that the winners have not yet been announced for “Putting the Glee in Gleason” contest.
I apologize but my partner in comedy has had some personal issues to deal with and I am swamped with school work. But the winners should be announced soon. Promise.
Yes, you can laugh at prostate cancer, BPH, etc.
By Howard Wolinsky When George Burns played God Almighty in “Oh,God!,” the 1977 movie, he was asked what mistakes he had made. He listed ostriches, tobacco, giraffes, avocados (“Did you see the size of the pits?), and, finally, as the story goes, the prostate.
Recommended reading
Keith Holden is a physician sharing his advanced prostate cancer journey at “Prostate Cancer Secrets.” He talks about PSAnxiety, financial toxicity, and other topics of interest to all of us on this path. Check him out at