Researchers recommend patients be counseled about potential long-term adverse effects before aggressive PCa treatment AND before PSA screening
Don't miss the ASPI, TheActiveSurveillor and Dr. Geo webinars
By Howard Wolinsky
High risks from erectile dysfunction and incontinence occur in patients undergoing aggressive treatment for prostate cancer, researchers report in a new study published on Nov. 7 in JAMA Oncology
The researchers from the Southwest Oncology Group (SWOG) contend that given the uncertain benefit of prostate cancer treatment for most patients, their findings highlight the importance of patient counseling before treatment and even before screening with PSA (prostate-specific antigen) blood tests.
Biostatistician Joseph Unger, PhD, of SWOG Statistics and Data Management Center, Fred Hutchinson Cancer Center, Seattle, Washington, and colleagues found the 12-year hazard risk of urinary (incontinence) or sexual complications (erectile dysfunction) was 7.23 times greater for those who had undergone prostatectomy and 2.76 times greater for radiotherapy compared to the untreated control group.
(Joseph Unger, PhD)
The researchers said: “This cohort study found that, even after accounting for age-related symptoms and disease, PCa treatment was associated with higher rates of complications in the 12 years after treatment. Given the uncertain benefit of PCa treatment for most patients, these findings highlight the importance of patient counseling before PCa screening and treatment and provide a rationale for pursuing opportunities for cancer prevention.”
3,946 participants had prostate cancer, 655 were treated with prostatectomy and 1,056 with radiotherapy. Participants included patients who had been diagnosed with prostate cancer but had not received treatment and were on Active Surveillance along with those who had not been diagnosed with prostate cancer served as an untreated control group for comparison.
For both treatment groups, the research team examined Medicare claims data for instances of 10 potential treatment-related complications and adverse effects: urethral stricture, placement of an artificial urinary sphincter (for severe incontinence), placement of a penile prosthesis, urinary incontinence, erectile dysfunction, radiation cystitis, radiation proctitis, bladder cancer, bladder cancer followed by cystectomy, and rectal cancer.
Unger told me: “In our model, all men started as untreated. Those who developed prostate cancer and received prostatectomy or radiation therapy were considered treated. Otherwise, all other men remained untreated. This included those with a prostate cancer diagnosis who never received prostate cancer treatment, and those who never developed prostate cancer at all (which was the largest group).”
Those in the prostatectomy group had a 12-year risk of having at least one of these 10 complications that was more than six times (6.57) greater than the risk faced by untreated participants.
For men in the radiotherapy group, the 12-year risk of experiencing at least one of the 10 complications was 3.04 times greater than it was for those who had not been treated.
Among participants treated with radiotherapy, there was a nearly 3-fold greater hazard risk of bladder cancer than in the untreated (hazard ratio [HR], 2.7), as well as an approximately 100-fold increased hazard risk of radiation-specific outcomes including radiation cystitis (HR, 131.47) and radiation proctitis (HR, 87.91).
So if you’re undergoing PSA testing, or are newly diagnosed with prostate cancer, discuss this study (https://jamanetwork.com/journals/jamaoncology/fullarticle/2826069?resultClick=1) with your urologist or radiation oncologist. Ask them their personal complication rates.
“This study throws down a major gauntlet to all physicians to give patients this information before they even begin the process of drawing a PSA test,” said senior author Ian Thompson Jr., a urologist with the University of Texas Health Science Center at San Antonio.
(Dr. Ian Thompson Jr.)
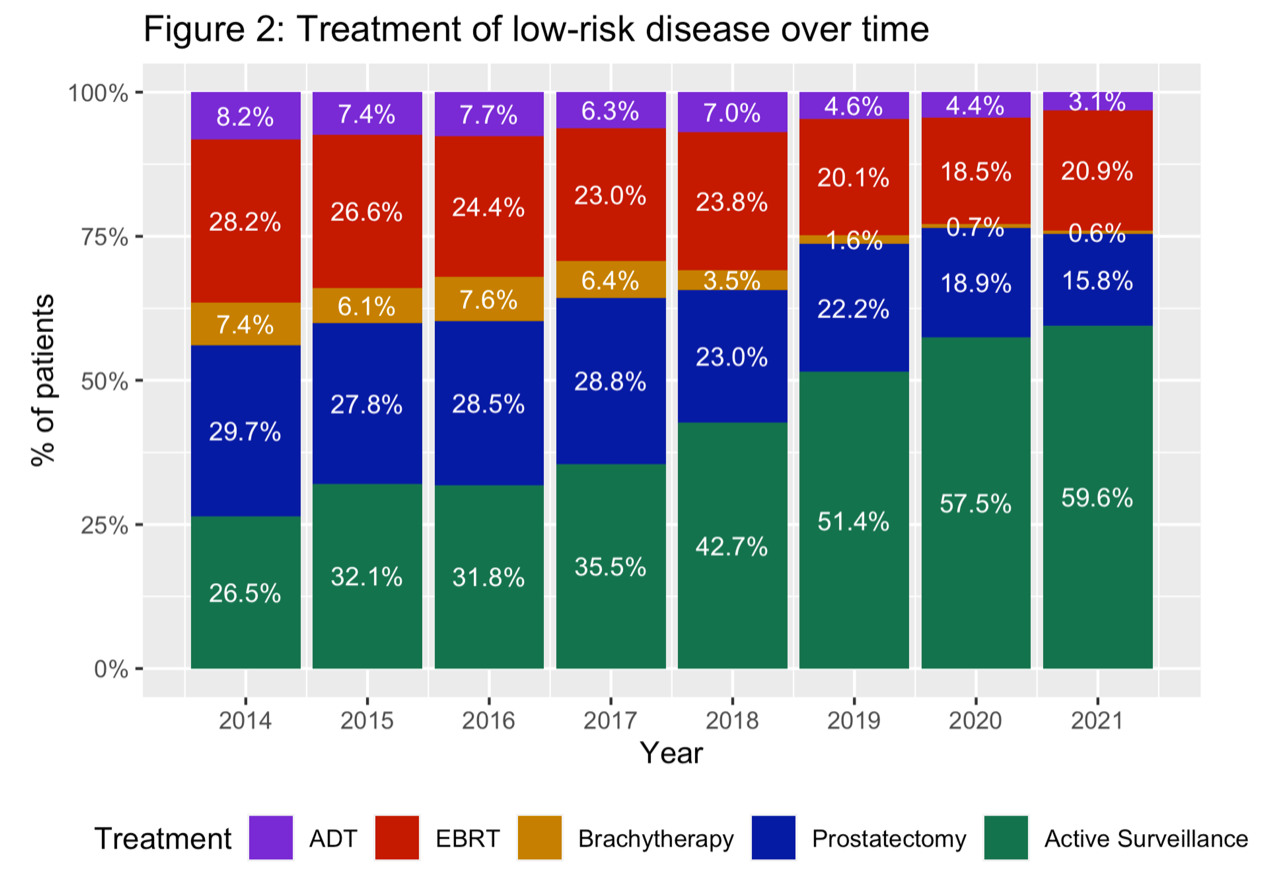
In the United States, per the American Urological Association ‘s (AUA’s) AQUA database), 40% of low-risk (Gleason 6/Grade Group 1) patients opt for aggressive treatment. There may be a variety of reasons: fear of not treatment the disease, emotional distress, such as anxiety—though guidelines from the AUA and the National Comprehensive Cancer Center Network recommend surveillance as the No. 1 option for patients with GG 1.
Compare AS uptake rates elsewhere: only ~ 10% of Gleason 6 patients in the state of Michigan opt for treatment and fewer than 5% do so in Sweden and the United Kingdom.
Only 20% of those with favorable intermediate risk (Gleason 3+4=7 or GG 2) opt for surveillance in the United States. In Michigan, 45% of these patients choose AS, a rate that may lead the world.
Keep in mind that more than 50% of those who choose surveillance drop out within five years of diagnosis. Why? Progression of the cancer, patients may be exhausted by the AS rigamarole, and stress of monitoring, and high anxiety or other emotional stress.
Daniel Spratt, MD, chair of radiation oncology at University Hospital in Cleveland, said “the new paper largely concludes that surgery has way more complications than radiation.
“However, this is a very flawed study from retrospective observational data. Remember that radiation patients are older and have more health problems at baseline than surgery patients. So the complication rates and secondary cancer rates would look even worse for surgery patients if these were from a randomized trial like ProtecT. Older patients get more cancer even with no treatment and have more other issues. This is why these same observational studies show that surgery patients live longer than patients without prostate cancer even It is because the selection bias of patients chosen for surgery.”
He stressed: Active Surveillance will always have lower side effects than any treatment, and should be done for patients it is safe to do.”
Unger et al. conclude: “Informed patient decision-making should include a complete understanding of treatment adverse effects. Most previous reports of adverse effects are limited to selected domains (eg, urinary, sexual), present single or limited institutional outcomes, or do not provide a comparable control group. This study aimed to characterize long-term treatment-related adverse effects and complications after prostatectomy or radiation therapy in the follow-up of 2 large PCA prevention trials.”
Unger told me: “Our aim was to better ensure that men with a prostate cancer diagnosis and their physicians discuss not just the possible benefits of prostate cancer treatment, but also the risks. It was our view that these risks had not been well characterized in a systematic fashion over the long term, and in a manner that accounts for the occurrence of many of the complications in the normal (non-prostate cancer) population.
“In fact to our knowledge, no national organization currently includes quantitative information on prostate cancer treatment-related risks and benefits. Our hope is that our findings are included in the care guidelines that inform the conversations between patients and their providers about what kind of treatment men with a prostate cancer diagnosis receive, or whether they choose to receive treatment at all.”
(Emphasis added.)
For the record, per the AUA’s Aqua database, prostatectomy has fallen by about 50% and EBRT (external beam radiation therapy) by about 10% in recent years as Active Surveillance has more than doubled.
ASPI presents: How you can help advance research on Active Surveillance
By Howard Wolinsky
Without clinical trials, such as ProtecT, patients with lower-risk prostate cancer would have had no choice other than aggressive treatment with risks of side effects impacting their quality of life. I have participated in about a dozen trials as a patient and a patient researcher.
I highly recommend participation in trials. I have been in studies on diet and low-risk prostate cancer, genetics and medications and low-dose aspirin and preventing heart attacks.
Look for trials on Active Surveillance that you potentially can join at ClinicalTrials.gov
Active Surveillance Patients International (ASPI) is holding a webinar at 12:00PM ET Saturday, November 30, entitled “How you can help in clinical research on Active Surveillance.”
REGISTER HERE: https://zoom.us/meeting/register/tJIocOCupz4jGtX8fHJ036bYGHYIjLfwfRzk
Speakers will include Kevin Shee, MD, PhD, a researcher at the University of California, San Francisco, and Mike Scott, founder of Prostate Cancer International and an early advocate for Active Surveillance.
Dr. Shee has been involved in multiple studies, the most recently one on whether men 75 and above should stop active surveillance.
Though not a prostate cancer patient himself, Mike Scott was the founder of one of the first support groups for men on AS. ASPI this year presented him with its 2024 Thráinn Thorvaldsson Award for Patient Advocacy.
A question-and-answer session will follow the presentations.
If you have questions, please send them to: contactus@aspatients.org
Climbing Dr. Geo’s ‘Prostate Cancer Summit,’ addressing AS, herbs, diet, prostate massage, and more
By Howard Wolinsky
Dr. Geo Espinosa (you may know him as the author and podcaster “Dr. Geo,”), the naturopath specializing in prostate care on faculty at New York University, is hosting a free week-long “Prostate Cancer Summit” you shouldn’t miss.
The free event runs November 19 - 25, with an “encore weekend” November 29 - December 1, 2024. Register here: https://drtalks.com/summit/prostate-cancer-summit/?uid=814&oid=83&ref=4266
(Dr. Geo)
Geo interviewed about 40 experts on prostate cancer—plus me. The interviews cover a full range of prostate cancer topics.
Speakers include urologist Dr. Stacy Loeb of NYU, on lifestyle; Dr. Sanoj Punnen of the University of Miami, on the value of MRI and biomarkers in diagnosing prostate cancer; Man Up podcaster Justin Dubin, MD, on regaining sexual health after treatment; Donald Abrams, MD, on marijuana’s role in prostate cancer management; and Eric Yarnell, ND, on herbs and PCa.
Geo interviewed me about Active Surveillance.
Register here: https://drtalks.com/summit/prostate-cancer-summit/?uid=814&oid=83&ref=4266
Find me here. Who else do you know?







I think that PSA is more misunderstood than misused. So many jump into a biopsy based on a PSA when the data they really needed was age, volume and genetics (SelectMDx). They just need to drop the DRE and start picking up the U/S probe. Following that, MP-MRI.
No need for a needle or scalpel until all the data is in.
Took me awhile to "skate in." Whether readership of this blog agrees or disagrees with your comments Dr. Vorstman, believe we are listening. I encourage you to continue to share.