By Susan Bottles with Kim Bottles
January 2020 was the first time my active, fit husband Kim, 71, heard the words, “It’s cancer.” Nearly exactly three years later, this January, he heard them again.
Different cancers, different treatment decisions, but Kim says, “Cancer is cancer. It is what it is, and you don’t have a choice but to deal with it the best you can.”
Kim’s first cancer was very rare male breast cancer. It strikes only some 2,800 men annually in the United Sates and kills about 530 of them. Only 0.6 percent of new breast cancer is diagnosed in men.
The diagnosis came as a shock.
(Kim and Susan Bottles.)
Not so shocking were the results of Kim’s first prostate biopsy this January: Group Grade 2, 3+4 Gleason score 7 in two cores, Grade 1 in an additional one. His prostate-specific antigen (PSA) blood level had climbed from 5.9 to 9.1 in 2022, prompting the biopsy.
So one man, who didn’t even take prescription medicine three years ago, now has both of the most common cancers, behind lung cancer.
Male breast cancer is so rare that Kim has yet to meet a fellow patient. It sometimes seems half of his friends have a story to share about their prostate cancer. Most people, men and women, are far more curious about the breast cancer, once they get over their surprise that a man can even get it.
Kim has always been very open about his diagnosis, never feeling it’s a “female cancer,” because, obviously to him, he is not female. He considers it a kind of public service to let people know, yes, men can get breast cancer, too, and what to look for.
Men are usually diagnosed with a more advanced stage of breast cancer than women because they are not screened with mammograms and not trained to look for lumps in their chests.
In his case, his left nipple began to invert and hurt over a couple of days. There seemed to be a lump underneath. We were just watching it until his massage therapist told him to see his primary care provider. His doctor said it was most likely an infection, but in addition to prescribing an antibiotic, he also scheduled a mammogram and ultrasound in a couple of weeks.
The next week at an ordinary skin check, his dermatologist noted the lump was still there. “I can reach that with a punch biopsy if you want,” she said, and did. A week later he got the cancer call, and the whole breast cancer protocol started to roll at our health maintenance organization, Kaiser Permanente. It was just weeks before COVID-19 threw health care into chaos.
Next up was a mammogram. Kaiser facilities are completely gender-neutral, but it was probably no coincidence no women were in the waiting room.
Skilled technicians can handle male mammograms, but Kim’s told him he was only the third man she had seen in 30 years with confirmed breast cancer. The follow-up ultrasound revealed enlarged underarm lymph nodes matted together, with a suspicion of “locally advanced” or Stage 3 cancer.
(The male radiologist was the only provider in three years who appeared uncomfortable, but that could have been just his stiff personality.)
Other testing revealed no metastases.
So, treatment. This is where the tale of the two cancers dramatically diverged. As I am a 10-year survivor of breast cancer, we already had a long-term trusting, caring relationship with a medical oncologist. We turned to him, just as we did again this year for evaluating options for Kim’s prostate cancer.
“Without breast-cancer surgery, your chances of survival are zero,” he told Kim. That does concentrate the mind. No choice, no waiting. After the mastectomy, he recommended the most aggressive chemotherapy followed by whole chest radiation.
Our path for the next 11 months was set, and strangely the fact the whole world was shut down with COVID possibly made losing that year easier. In the end, Kim now has an 85 percent chance of survival.
So few male breast cancer patients means clinical trials are impossible. Men are treated the same way as women, although tumor biology differs, as, of course, does the whole body. But males overwhelmingly have estrogen-sensitive tumors (yes, men make estrogen, too). Kim now takes the estrogen-blocker Tamoxifen, as do most premenopausal female survivors. Side effects are manageable.
Kim has no known risk factors for either cancer except for his mother with breast cancer. There can be a genetic link, including with prostate cancer, but testing after both cancers found he had no suspicious mutations.
As a male, Kim was spared the kind of devastating psychological overlay women experience with breast cancer. He had seen that firsthand when I had invasive cancer in both breasts and a double mastectomy. He has great sympathy for the women, who also uniformly have shown great sympathy for him and welcome him into the “sisterhood.”
Breast cancer decision-making was clear-cut. Not so with prostate cancer. Kim says he finds the uncertainty of prostate cancer much more challenging. He has neither anxiety nor depression, but he does want to avoid possible long-term treatment side effects if possible.
Kim’s business partner has been in a long-term clinical trial of active surveillance for Gleason 6 prostate cancer. He shared Dr. Mark Scholz’s books and online resources. We self-educated, with no guidance from Kim’s urologist, with whom Kim has only talked by telephone except during the biopsy.
The urologist recommended against prostatectomy and suggested possibly simply living life as it comes. Kim’s younger brother, Kent, a medical doctor from the Philadelphia area, prescribed the same approach.
The urologist did not mention AS but was OK with AS when we brought it up. He also scheduled consultations with a radiation oncologist.
We discussed the biopsy results with our medical oncologist--we share the same one-- and his radiation oncologist. They both favored treatment as they both wanted to rid his body of “cancer.” But they both agreed that AS was a reasonable option as long as we watched my situation carefully and acted quickly if we found any sign of PC aggression.
Both the radiation oncologist and our medical oncologist also agreed that while active surveillance is feasible for now, Kim he is a borderline candidate. Waiting might mean intensified treatment later. The Decipher genomic test also stated his “low intermediate-risk of metastases following either radiotherapy or prostatectomy,” make him “not an ideal candidate for active surveillance.”
If any parameter advances, our medical oncologist said he will recommend treatment. “I’m a cancer doctor. I don’t want cancer in my patients’ bodies. We can not know when it might metastasize. It can be cured now,” he said. He projects Kim’s life expectancy as possibly 15 or 20 years.
Kim’s brother, a retired pathologist, says every autopsy he did on elderly males found prostate cancer cells. He recommends against PSA testing and advocates ignoring the whole thing.
For now, Kim’s choice is active surveillance. \
Susan Bottles has a degree in journalism and has spent time as a writer and community newspaper reporter. She has also done extensive community volunteer work. Kim has a degree in business majoring in accounting. He has worked as a CPA in public accounting and also as a financial executive in private industry. In 1994 he and a partner purchased a midsized commercial general construction company from which he retired at the end of 2014.
The Bottles have been married for 55 years and have two grown sons and one granddaughter. They live on Bainbridge Island across Puget Sound from Seattle.
Susan is interested in reading, volunteer work, and travel. Kim has been a bicycle racer, ham radio operator, and sailboat racer. The Bottles cruise the sailboat and a motorboat on the Salish Sea.
Men with breast cancer face special challenges
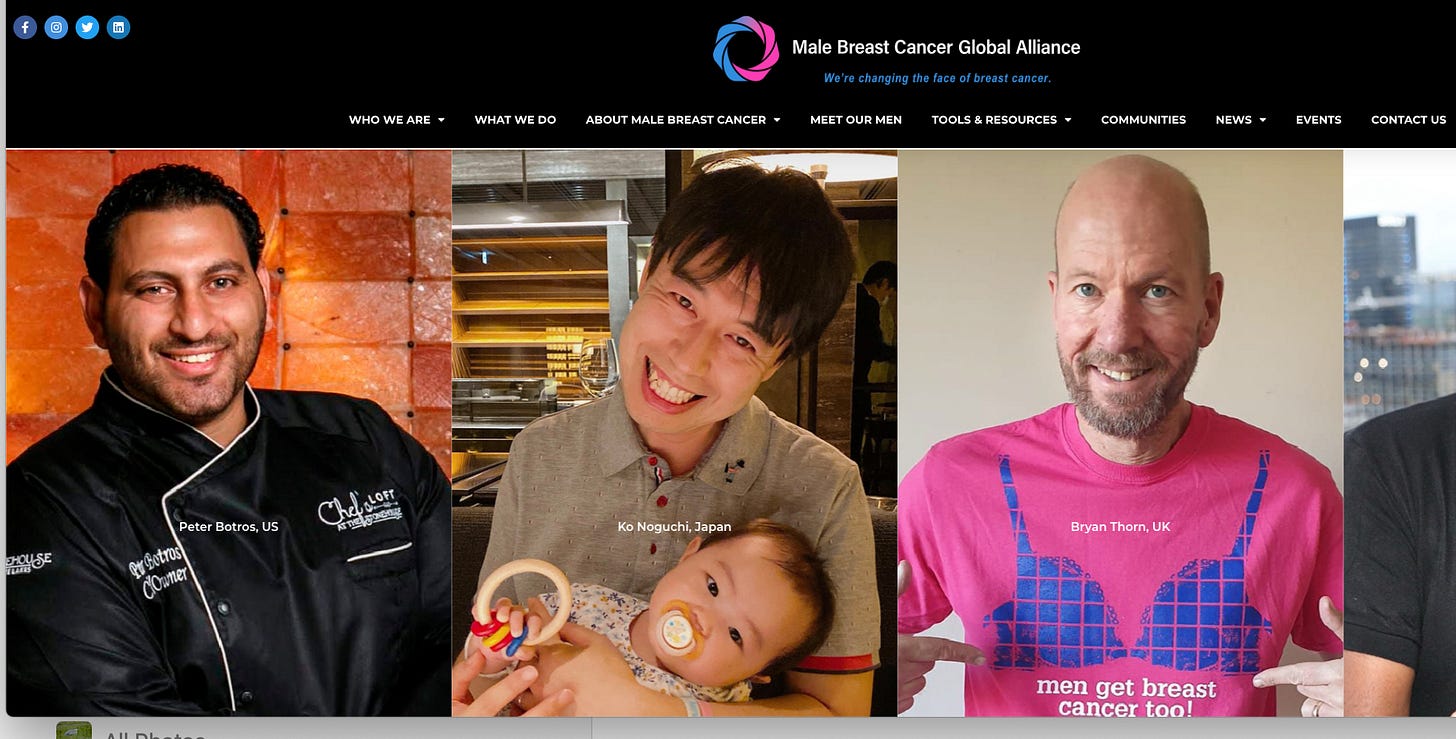
By Cheri Ambrose/ Founder/president Male Breast Cancer Global Alliance
Men for the most part are not ones to run to a doctor.
When they do, oftentimes, they are met with ignorance from primary care doctors who have handed men topical cream and told them to come back if the lump doesn’t go away or the nipple doesn’t stop leaking.
Several have been met by intake staff members at breast centers who ask if they are there for their wives.
As you can well imagine, these actions are very discouraging.
Sadly, the stigma of breast cancer being a female disease is still very much a thing. Some men choose to keep their diagnosis to themselves while others seek support.
We find that those who connect with other survivors seem to have fewer body image and psychological issues.
The lifetime risk for men to be diagnosed with breast cancer is 1 in 833. While these numbers are low compared to women, the mortality rate for men is significantly higher. This is due in part to lack of awareness and/or misdiagnosis.
If the primary care doctors would simply pay more attention to family health history and perform breast checks on men during annual exams, more breast cancers may be diagnosed before they metastasize.
We have been successful in bringing men into more breast cancer clinical trials. Our Advocacy work was also one of the driving forces behind the labeling change to Pfizer’s metastatic drug, Ibrance, to include men.
Our hope is to see a man represented in a breast cancer drug commercial one day and are working with big pharma to help make that happen.
Knowledge is power.
https://mbcglobalalliance.org/
Back to class: Active Surveillance 101 takes on prostate imaging
Andres Correa, MD, urologic oncologist, an assistant professor of surgery at Fox Chase Cancer Center in Philadelphia, is presenting a program on prostate imaging in the Active Surveillance 101 series. The free program is on at noon Eastern, Saturday, May 27. REGISTER
If you have questions, please send them to Mark Lichty at mlichty@aspatients.org. Dr. Correa is unable to attend but will try to answer questions in a separate video.
The AS 101 series was created to provide newbies, those in the “grey zone,” and even veteran patients with video covering the basics of AS when no other help is available. Patient Larry White and his well-informed spouse Nancy will interview Dr. C. about mpMRIs and microultrasound, an emerging imaging technology.
ASPI, AnCan Virtual Support Group for AS, Prostate Cancer Support Canada, the Prostate Cancer Research Institute, and TheActiveSurveillor.com are co-sponors of AS 101.
The full AS 101 series to date may be viewed at: https://aspatients.org/a-s-101/





This just in from MedPageToday. My blof on lumpers vs. splitters with very low-risk prostate cancer: https://www.medpagetoday.com/special-reports/apatientsjourney/104586. More later,