Tale of two different 'animals': MRI-visible and MRI-invisible lesions
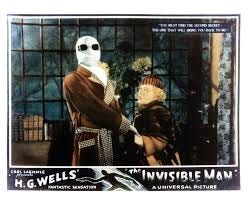
A patient story coming. And come to the ASPI webinar on January 25 with your cloak of invisibility if possible
By Howard Wolinsky
Consider two types of prostate lesions: MRI-visible ones and ] MRI-visible ones.
Has your urologist ever mentioned you have invisible lesions and that they are a good thing, akin to a Gleason 6 diagnosis? Some research is suggesting many of us have invisible lesions, which are taken as a positive sign.But as always, there are equal and opposite MDs and PhDs arguing the case,
Fact: Pathologists looking under their microscopes can see a cancer, one a radiologist might miss simply because it’s too small and beyond of the the capabilities of MR imaging.
Dr. Mark Emberton, director of interventional oncology at University College London and Dean of its Faculty of Medical Sciences, a pioneer in prostate MRIs, is among a growing group of experts that consider the MRI-invisible lesions noncancers and a good sign for patients, akin to Gleason 6, even the pathologist has identified cancers up to Gleason 7 or 8.
[Note: Dr. Emberton will be featured at ASPI’s web on Saturday, January 25, 2025, from noon – 1:30 p.m. Eastern (5:00pm-6:30pm UK time).
Don’t be invisible. Register here: https://zoom.us/meeting/register/tJYldu-qqzojGNEzCkgPQuTOWYGhcL80Dhec']
(Check out my article on invisible lesions in Medscape: https://www.medscape.com/viewarticle/mri-invisible-prostate-lesions-are-they-dangerous-2025a10000cw)
“The evidence is not perfect because it's early days. But actually, the evidence that is out there, which everybody can read, suggesting that these are very, very different animals as you would expect, yeah?” said Emberton.
“A visible nodule, a visible cancer, never goes away. It progresses. It's just a case of when. We have no idea what the fate of invisible disease is. Some of it may indeed go away. We just don't know, because we can't measure it. And when we rebiopsy somebody, you can't find it again. Or you find more disease, but you don't know whether you're hitting the same bit, or you're just finding another bit of cancer that you missed on the first go.
“So if you can't see it, if you can't measure it, I would argue that you can't do science on it. And I'm not alone in that. Lord Kelvin said the same 200 years ago.”
[Scottish-Irish physicist William Thomson, better known as Lord Kelvin, was one of the most eminent scientists of the 19th century and is best known today for that bears his name for inventing the international system of absolute temperature.]
Emberton noted that prostate cancer has always been diagnosed in a different fashion from other solid cancers, such as of the lung, liver, kidney, or brain. He said doctors don’t mention cancer in these cases unless the patient has been diagnosed with a visible cancer.
“If you look at all other solid organ cancers, all of which are much more aggressive and much more lethal than prostate in terms of the likelihood of surviving if you're diagnosed with one, they're all visible lesions. So, they exist when you can see them,” he said. “If you have a headache, and you're worried about a brain tumor, you have a scan. If your scan is normal, nobody sticks a needle in your brain.”
Emberton said urologists have “a habit of sticking needles into normal-looking prostates, because before ultrasound and MRIs, and now PSMA PET, they had difficulty imaging the tumor.”
Emberton argues that if you can’t see it on MRI, then it’s not cancer. He doesn’t subject such patients to biopsies. “I don't biopsy healthy tissue,” he told me. So he doesn’t estimate the incidence of MRI invisibility.
While Emberton doesn’t biopsy invisible lesions, some other doctors have and can estimate the presence of invisible lesions:
—Dr. Laurence Klotz, of the University of Toronto, one of the developers of Active Surveillance in the late 1990s, estimates that invisible lesions are present in about 20% of patients with favorable intermediate-risk (Gleason 3+4=7). “Looking beyond Gleason scores for risk prediction, MRI “visibility is a very powerful risk stratifier,” he said.”
— Dr. Christian Pavlovich, head of the Active Surveillance program at Johns Hopkins, told me: “hat percentage of the patient population are they? 50% of men in our AS program have negative MRIs. Some might say they never should have been biopsied… but some have very high PSA, PHI, GG2 disease, large volume disease, etc so I stand by diagnosis when suspicion of higher grade disease exists.”
Klotz said, “Several active surveillance cohorts have shown that the patients with invisible cancers on surveillance do drastically better than the ones who have visible cancers.The message is that invisible cancers have favorable genomics. They have an indolent natural history. You don't need to find them.”
Klotz said the concept of invisible lesions has been gaining traction recently with the emerging field of radiogenomics, correlating gene alterations in the tumor tissue and MRI invisibility.
He reported in the September issue of the Journal of Urology (https://www.auajournals.org/doi/full/10.1097/JU.0000000000004069) that recent radiogenomic analysis revealed that the genetic aberrations that account for tumor visibility on MRI are the same mutations linked with cancer invasion and metastasis. He said the implication is that invisible cancers are “genomically and clinically indolent and benign in their behavior.”
He said this means that invisible cancers are clinically insignificant and don’t require systematic biopsies.
In an editorial in the journal, Todd Morgan, MD, chief of urologic urology at the University of Michigan and a prostate genomics researcher, said: “The idea that MRI visibility correlates with disease biology is incredibly appealing.” [https://doi.org/10.1097/JU.0000000000004069]
But the Michigan researchers xsaid: “The genomic difference in visibility and invisibility is tied to a group of genes involved in cellular organization and structure; this has obvious biologic plausibility and is highly accurate in separating visible from invisible tumors. These genes are notably not correlated with disease aggressiveness. The factors that distinguish radiographic conspicuity don’t predict meaningful cancer outcomes.”
Morgan said Grade Group 1prostate ca ncer can be safely watched because it has practically no metastatic potential and does not cause prostate cancer death. He said the management of MRI-invisiblity as if it were the same as Gleason 6 has not been established.
Pavlovich told me at January 4 webinar, “Active Surveillance 2025: The Year in Review,” that MRI can simply miss very small lesions.
He said: “So then we show the radiologist and say, was this really not there on the MRI three years ago? And they say, actually in retrospect, I see something there. So then is it really invisible? Was it invisible? Or was it just underappreciated?”
Pavlovich said: “[This is] still a developing field. It's certainly better to have an MRI that appears normal than one that doesn't, but it's not the be all and end all. And sometimes, you can catch very high-grade small lesions not seen on MRI affect a cure with radical prostatectomy or radiation and really cure the Gleason 8 patient, whereas if you waited till it became MRI visible, and it went high-grade, that would not be as curable.”
Dr. Brian Helfand, chief of urology at NorthShore University HealthSystem outside Chicago, told AS 2025, ‘MRIs have moved the bar significantly, but they are still not perfect. And again, well, they have their limitations.
“I always target visible things that we can see, but also the kind of invisible areas as well on biopsies is because about 30 percent of patients will be upgraded in the -- or more aggressive tumors in that invisible area.”
[Note: The video from “AS 2025: The Year In Review” will be available soon.]
The invisibility theory is subject to plenty debate.
Biostatistician Andrew Vickers, PhD, of Memorial Sloan Kettering Center Center in New York, said, “I 100% agree with [Emberton] that MRI visibility is a strong prognostic factor, I just disagree that it is perfect. It is widely known – and has been published – that you can get very high-grade cancers - grade group 4 and 5 - in men with negative MRI. Again, sensitivity of MRI is very high for these sorts of cancers, but it is not perfect. My own guess is that the sensitivity for MRI for the most aggressive cancers is somewhere around 95% in good centers, close to 99% in the best centers but perhaps 85 – 90% in routine care.”
Drs. Todd Morgan, chief of urologic urology at the University of Michigan \ (Go Blue!) and a prostate genomics researcher, and Patrick Lewicki said: “The idea that MRI visibility correlates with disease biology is incredibly appealing.”
They said: “The genomic difference in visibility and invisibility is tied to a group of genes involved in cellular organization and structure; this has obvious biologic plausibility and is highly accurate in separating visible from invisible tumors. These genes are notably not correlated with disease aggressiveness. The factors that distinguish radiographic conspicuity don’t predict meaningful cancer outcomes.”
Researchers at Cedars Sinai Medical Center in Los Angeles associated cancer invisibility and certain mutations. These include four genes (PHYHD1, CENPF, ALDH2, and GDF15) that predict MRI invisibility and are associated with worse progression-free survival and metastasis-free survival. They said: “It is possible that tumors visible on MRI are simply high-grade tumors.” [https://www.thno.org/v08p1752.htm]
The UMich researchers said Grade Group 1(Gleason 6) prostate cancer can be safely watched because it has practically no metastatic potential and does not cause prostate cancer death. They said the management of MRI-invisiblity, as if it were the same as Gleason 6, has not been established.
Check out the first edition of my Prostate Cores Substack newsletter linked here. Why not subscribe? Keep up to date with low-risk prostate cancer, BPH, cancer survivorship.