Part I Transrectal biopsies? Avoid them at all costs, Canadian prostate expert tells webinar
TPs in the office v. the OR: another debate
(Editor’s note: I have written a lot and talked a lot about transperineal biopsies. In my mind, they offered patients safety from sepsis and the bad biopsy stewardship that contributes to the crisis with antibiotic-resistant organisms. It can be performed in the doctor’s office without IV antibiotics and with only local anesthesia. But I have been hearing about men who opt for TPs in the OR with general anesthesia and IV anesthesia. Also, at all costs, avoid random biopsies. Shots in the (very) dark. Best to have MRI findings guide biopsies.)
By Howard Wolinsky
No ifs, ands, or buts about it. Men should opt for transperineal biopsies, a leading Canadian doctor told a webinar this week.
Danny Vesprini, MD, a radiation oncologist and head of Active Surveillance at Sunnybrook Health Sciences Centre at the University of Toronto, said, “There should be no transrectal biopsies” because of the risk for infections, such as sepsis.
Vesprini was speaking to a webinar co-sponsored by the Walnut Foundation and Prostate Cancer Support Canada. To view the program, go to Prostate Cancer Support Canada’s website.ca
Vesprini, an assistant professor in the department of radiation oncology at the University of Toronto, said his program exclusively uses transperineal—no general anesthesia and no IV antibiotics. Let me repeat: No general anesthesia, just local. And Zero antibiotics.
How did you do your transperineal?
Doctors and patients in the United States are divided on this issue. Many patients and some doctors say transperineal biopsies are the way to go.
But few U.S. docs perform transperineal biopsies. About 5% of the 2 million prostate biopsies in the U.S. are done transperineally, while some countries have in effect have banned transrectal biopsies.
The AnCan Virtual Support Group for Active Surveillance and Active Surveillance
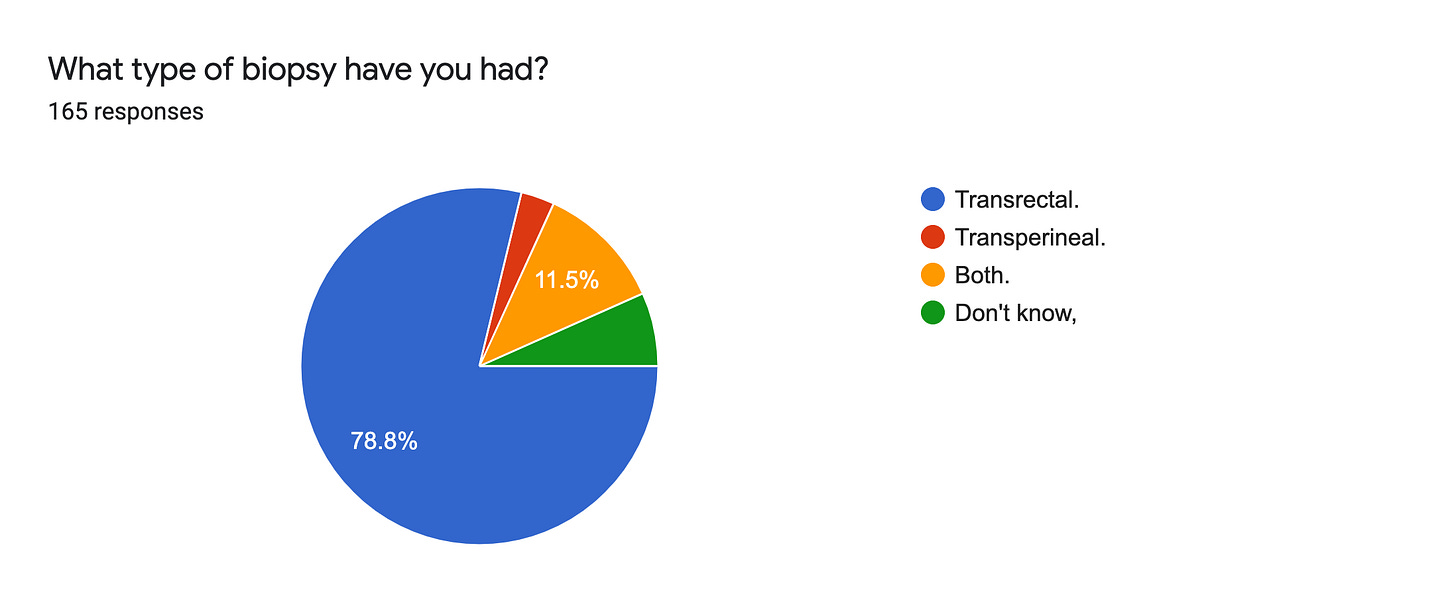
Patients International found in a survey of 165 men we conducted last May that 17% of them have had transperineal biopsies. So we’re a more sophisticated audience.
But I am starting to see a pattern within those who had transperineal procedures.
Some patients—and their doctors—prefer the patients being knocked out in the OR and administering IV antibiotics, which adds to the sepsis issues we face as patients, with bacteria becoming increasingly antibiotic-resistant.
Vesprini stressed, “We don't even use antibiotics when we do transperineal biopsies (TPs).”
Many men (one-third) in the AnCan-ASPI survey said their urologist never warned them about the risk of sepsis and other infections.
How TPs are performed
TPs involve needles entering through the taint—the space that ain’t the testicles and ain’t the anus, as the RadOnc said. The skin is cleansed. And germs are avoided in the dirty rectum from the transrectal procedures, which involve the doctor navigating through the rectum, or ”back passage,” to use a biopsy gun to extract prostate samples for biopsies.
Inexplicably, to me anyway, some doctors insist on IV antibiotics in OR-based transperineal biopsies. I thought the point of all of this was to steer clear of antibiotics and general anesthesia.
Is this to increase revenue from transperineal biopsies? Is this for malpractice insurance reasons?
Admittedly, biopsies make some men so jittery that they prefer the OR and anesthesia to transperineal biopsies even though the pain from TPs is reported by patients to be only slightly higher than that from transrectal ultrasound (TRUS) biopsies.
(I plan to write more about this soon.)
(Disclosure: I haven’t had a transperineal biopsy. I haven’t had any biopsy in nearly six years and am monitoring with the PHI (Prostate Health Index) blood test. My doctor had said I most likely am done with the biopsy assembly line and even getting off the MRI train. I will be 75 this year. For years, experts have told me to stop biopsies. You have to get advice from your own urologist.)
Radiation oncologists like Vesprini are accustomed to using steppers in performing brachytherapy with templates.
In the treatment of cancer, especially prostate cancer, radioactive implants are implanted directly into the tissue following a template pattern. In the case of biopsies, the same gear can be used to insert needles to extract biopsy samples, or cores, maybe dozens, in transperineal procedures. There are other ways to perform TPs.
RadOnc Vesprini said his group has partnered with the urological community in Toronto.
“We taught them how to do [transperineals], and that's all they offer,” he said.
Vesprini noted that transperineal procedures predate transrectal biopsies. He said the urologists are indeed “reluctant to change.”
He urged patients to “put pressure on your urologists because they should learn how to do it because it's one safer and it's okay with you.”
Changing med practice? Taint easy?
Vesprini noted: “It is very hard, particularly with stubborn doctors, to change how things are done because there's always a resistance, because this is the way the way we have done for years, and it works.”
My observations are that:
—Urologists believe they are not putting patients at risk;
—They feel transrectal is just as safe as transperineal biopsies;
—They believe transrectal procedures can hard-to-reach places that often are sites for cancer;
—They don’t want to go through retraining (a waste of time in their minds);
—And they don’t want to invest $40,000 to do a safer procedure on their patients.
Vote with your feet—and your prostate
Vesprini suggested that patients with all manner of prostate issues who want transperineal biopsies tell their resistant doctors: “I'm going to take my business elsewhere … I mean, it's a business.”
Patients in Norway and Australia have voted with their feet—and prostates—by switching to doctors who do transperineal biopsies. I have written about this before.
[The Norway story: https://howardwolinsky.medium.com/death-by-prostate-biopsy-5b5bb9c0bf5a
[The Australia story: https://howardwolinsky.medium.com/the-movement-to-make-transrectal-biopsies-go-extinct-e6e16538769f ]
Eventually, Vesprini said, doctors will conclude: “We’d better learn how to do this because we're losing all our business, right? I mean, it really is at the end of the day it's just like anything else.
Biopsies and McRib sandwiches: You deserve a break today
“If you wanted to pressure, McDonald's to bring back the McRib, you're gonna say if you don't bring back that McRib, I'm going to Burger King, and eventually they'll bring back the McRib.”
NOTE: Vesprini said he has never had a McRib. And he doesn’t recommend them. They were mentioned for illustrative purposes. Personally, when they come back, I might indulge. But that’s another story from here on the wild side.
Can you, meanwhile, vote on in-office transperineal biopsies with only local anesthesia and no antibiotics vs. OR-based transperineal with general anesthesia and IV antibiotics: https://www.surveymonkey.com/r/D2J8XY9
Please sound off in the comments below. I want to hear your point of view. After all, this is your taint I’m talking about.







From the information I gleaned from the ASPI presentation on TP biopsy, I knew to ask for TP if and when a new biopsy was needed. My annual MRI indicated a new "area-of-concern"; so I insisted (voted) that it must be a TP. And because of the MRI, it needed to be a Fusion. Which means it would need to be done under GA. My current Urologist, Dr. Cochran-Dallas, supported my decision and was the referring physician to get me to Dr. Walsh in NE Texas. Dr. Walsh uses the Matt Allaway device.
The TP was a more positive exercise than the TRUS I had 3 years ago. By at least a universe!
Yes, I voted with my prostate.
Yes, I'm an experienced advocate for TP.
Yes, I got a much more accurate/improved data set about what is happening and where it is happening in my prostate
Yes, no infection; and better recovery in all urinary and sexual aspects.
Background: Original biopsy was standard TRUS since I was uninformed and didn't know better. 1 year of infection, prostatitis, and general urinary misery until I got to Dr. Cochran who recognized the issue and got me healed through a more lengthy antibiotic regimen. I fired 3 urologists before I got to Dr. Cochran.
I've read that thicker gauge needles are required for TP biopsies because the perineal tissue is much thicker and denser than the rectum. Also, for the same reason, more force is required to traverse the perineal tissue and to keep the needle trajectory accurate. I wonder if pushing 10-20 thicker needles through the perineum may results in trauma, soreness or permanent injury to the prostate.