UConn's Albertsen selected for Chodak Award for trailblazing AS research
He helped show the way to Active Surveillance
By Howard Wolinsky
Active Surveillance Patients International (ASPI) presented its Chodak Award on July 6, 2023 to Dr. Peter Albertsen, one of the pioneers of Active Surveillance (AS), a noninvasive treatment strategy to manage low-risk prostate cancer.
Mark Lichty, chairman of ASPI, said, “Dr. Peter Albertsen was one of the earliest champions of AS. The urology establishment ostracized him in the 1990s and 2000s because he challenged the norms of managing patients with low-risk cancer and because his work did not come from one of the traditional centers of urologic research.”
Albertsen, of the University of Connecticut, who persevered and saw his ideas confirmed and become widely adopted, said: “My career has been spent trying to understand the impact of PSA [prostate-specific antigen] testing and the natural history and appropriate treatment of prostate cancer. Your award tells me that it has been time well spent.”
Today, AS has a 60% uptake among low-risk patients in the United States and over 90% in the UK and Sweden.
(Dr. Peter Albertsen and the Chodak Award)
The Chodak Award is named in honor of the late urology researcher Dr. Gerald Chodak, who, while at the University of Chicago laid down the intellectual framework for AS in the New England Journal in 1994. He was ASPI’s first medical adviser. ASPI is the first global support and education group for patients with low-grade prostate cancer.
Dr. Chodak was not only a noted researcher but also a painter and glassblower.
Glass artist Eli Zilke, of Benton Harbor, Michigan, was Dr. Chodak’s glass art teacher and donated the piece presented to Dr. Albertsen. It is the replica of a blue-and-white piece Dr. Chodak made.
Robin Chodak, Dr. Chodak’s widow, said, “The color blue was used for the bowl to represent prostate cancer awareness. Let the beautiful glass bowl award be a reminder for doctors to continue to utilize science and offer the best treatments to men with prostate cancer as Dr. Chodak always did.”
The first Chodak Award was presented in 2022 to Dr. Laurence Klotz, a University of Toronto researcher, one of the “fathers” of AS. Klotz, who considered Chodak his mentor, faced the same resistance to AS experienced by Drs. Chodak and Albertsen.
Howard Wolinsky, an ASPI co-founder and a friend of Dr. Chodak’s, said, “Dr. Chodak like Dr. Albertsen recognized that the impact of PSA testing had not been thoroughly evaluated through randomized trials and correctly anticipated an epidemic of overdiagnosis and overtreatment and a tsunami of adverse effects.”
The Chodak Award was presented in an online ceremony on July 6 and attended by Dr. Albertsen’s UConn residents.
ASPI previously gave a special award in June to MUSIC, the Michigan group that has increased the uptake to AS in low-risk patients to over 90%. Read about it here.
ASPI later will recognize co-founder Thrainn Thorvaldsson, who in Iceland started the first support group for AS patients,
(More to come.)
Recollections on Dr. Gerald Chodak
(Francis Fullam has been a neighbor and friend of mine for more than 30 years. He was a patient satisfaction expert at the University of Chicago and is now is an
Assistant Professor, Health Systems Management, Rush University Medical Center
in Chicago. Francis is worthy of a story in himself. But here he remembers another mutual friend, Dr. Gerald Chodak, for whom Active Surveillance Patients named its Award, honoring Dr. Chodak’s patient advocacy while the mainstream fought against his ideas for Active Surveillance.)
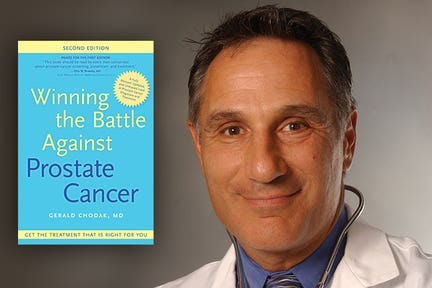
(Dr. Gerald Chodak.)
By Francis Fullam
So many stories and memories are shared about Dr. Gerald Chodak – I wanted to add my own to show more evidence of his vision, collaborative approach as a physician, and humanity.
In the 1980s and 1990s, when I was a hospital marketing and survey researcher, hospitals generally did not know much about their patients' needs, wants, and preferences – from their point of view. Providers generally felt they knew what was best for patients and patients themselves were not seen as valuable contributors to the design of medical care.
I was at the University of Chicago Hospitals in the early years of trying to understand the patient's voice. The Hospitals felt that the future success in providing care would involve getting feedback from patients about their own care. We participated in the early work of the Picker-Commonwealth project that eventually evolved into the national Hospital Consumer Assessment of Healthcare Providers and Systems (HCAHPS) patient survey.
Dr. Gerald Chodak had an established and growing urology practice at the University of Chicago Hospitals. He contacted me - “Call me Gerry” – for help with a patient survey he was developing.
That stood out to me for two reasons. At that point, not many physicians saw the benefits of systematically surveying patients to get their point of view.
I have found that sometimes physicians, in their drive to master so many technical fields, feel they can be experts in everything. Dr. Chodak was not one of those. He knew that he knew what he knew and was open to the expertise of others.
The other reason was that he immediately insisted I use his first name, another uncommon practice among faculty members in my experience.
In his work with the overtreatment of prostate cancer, he had a theory about a flaw in the patient decision process.
He explained the loop of miscommunications between physicians and patients. When a physician meets with a patient diagnosed with prostate cancer who wants to understand their surgical options, physicians will try to explain the probability of the risks of prostate surgery.
Physicians rely on their experience in asking prostate patients about their complications and on published reports on complication rates. In post-surgery follow-up visits, surgeons would directly ask patients if there were any complications.
Some complications are embarrassing to patients - urinary and rectal incontinence, impotence, etc.) - so patients can be reluctant to admit them or under-report their extent. Are they lying to their doctors? No, patients are just in a social situation where they might not want to embarrass the physicians or themselves by reporting complications from the surgery.
If they were based on physician reports of patient complications, published reports on patient complications would also underreport actual complications. Even if the physician did not ask the patients themselves about the complications rate, but had patients fill out a form in the physician's office, it would also underreport actual complications.
At the University of Chicago, I studied survey research and my graduate course with Norman Bradburn introduced me to the concept of "response effects". Patients were not lying to their physicians - but the situation of this particular interview had social dimensions that influenced how patients responded to the questions.
If physicians had more accurate tables of complications, the conversions that they had with patients considering surgery would be better informed and allow patients to make better choices. A patient who thought there was a faint chance of incontinence from the surgery – say less than 1 out of 100 – might think differently about the surgery if it were 1 in 10.
Gerry thought that if the situation of the interview about complications was more neutral (paper form mailed to the patient’s homes), patients might be more willing to be honest and report what actually happened. So we worked on a patient survey that would be sent to patients' homes after surgery. By changing the social situation, the setting where patients are reporting on complications, they might be more willing to admit the existence or extent of the complication. The survey research literature indicated that this might be the case.
I moved on from the University of Chicago Hospitals, so I do not know what happened with the survey. But it is another example of how Gerry was decades ahead of others in his field.
After all this time, my major impression was that he was a compassionate man who respected patients, understood potential biases that his colleagues were unaware of, and was willing to test his theories.
And such a nice, decent man.
Genomic guru to speak to AnCan in webinar on July 31
By Howard Wolinsky
Todd Morgan, MD, Chief of the Division of Urologic Oncology at the University of Michigan, is presenting a webinar for the AnCan Foundation at 8-9:30 p.m. July 31 entitled “How and why PCa genomic tests work ... What's Inside the Black Box?"
To register, go to: https://tinyurl.com/ancanpcagenwebinar
The program is aimed at the full spectrum of patients with prostate cancer, from low-risk to high-risk.
Morgan will cover the difference between inherited and somatic testing, who should undergo genomic testing, and his upcoming randomized trial comparing the leading genomic tests, Decipher, Prolaris, and Oncotype DX.
Please send your questions, comments and feedback to: joeg@ancan.org
Pissed off about a urinary issue?
By Howard Wolinsky
Active Surveillance Patients International has posted its July 1 webinar with Dr. Dean Elterman, of the University of Toronto.
Dr. Elterman is excellent.
The chances are very high that you’ll have a urinary issue by the time you’re 80. It’s not just an enlarged prostate. It can be an overactive bladder and more.
Elterman busted some myths.
For example, urinary symptoms rarely are linked with prostate cancer.
Also, you don’t need eight glasses of water a day to be hydrated. About half—or one liter—should do the job.
Handy for me since my wife often reminds me that I might be dehydrated, Four ounces is more doable.
Here’s the link: https://aspatients.org/meeting/pissed-off-the-many-ways-urination-can-go-wrong/
Optum Health launches a browser course on Active Surveillance
Optum Health, the Eden Prairie, Minnesota-based network of clinicians and physicians, has just launched a new online “browser course” to help Optum Health patients and the rest of us understand prostate cancer screening, biopsies, and Active Surveillance.
The free program, Prostate Watch Academy, which requires registration, is available at https://prostatewatch.thebigknow.com/home.
It is worth checking out, especially for those starting on PSA blood tests, those facing biopsies, and those making prostate cancer management decisions about Active Surveillance or close monitoring vs. aggressive treatment.
The course has a strong pro-AS message but shares the pros and cons of all options.
Also, check out Active Surveillance 101, an online video course from the Active Surveillance Coalition featuring leaders in the field: https://aspatients.org/a-s-101/
Check out a webinar on the future of Active Surveillance featuring Dr. Peter Albertsen, Dr. Laurence Klotz and other leading researchers on active surveillance: https://aspatients.org/meeting/your-voice-in-the-future-of-active-surveillance/




Congratulations Dr. Albertsen on receiving this award! As a PCa patient currently on AS, I wish to thank you and all of your colleagues for everything you have done in your careers to promote active surveillance. What a benefit it has been to countless men, including myself. Kudos!