Waiting for guidelines supporting transperineal biopsies in America? Is it akin to the absurdist play 'Waiting for Godot'?
Is a ray of hope about to appear? Read on.
By Howard Wolinsky
Since 2021, I have been campaigning for transperineal (TP) biopsies to replace germy and potentially dangerous transrectal (TR) biopsies.
(Rick Davis, founder of AnCan Foundation recently summarized my efforts: https://ancan.org/transperineal-prostate-biopsies/)
It’s been a quixotic journey—in America anyway—as U.S. experts wait for definitive randomized studies while European and Australian experts already adopted TP as the top choice.
One step forward, two backward.
A TR biopsy involves a urologist pushing biopsy needles through the germy rectum—and urologists prescribe countermeasures with antibiotics. This is creating a new problem: antibiotic resistance that helps germs get stronger and antibiotics lose their superpowers.
TP biopsies involve passing the needles through the perineum, the area between the anus and the testicles. European and Australian experts—along with a few U.S. experts—think TP is safer and will save lives and prevent antibiotic resistance.
I started my campaign with an article in Medium called “Death by Biopsy” and in Undark and Salon A common biopsy is putting lives at risk. It’s time to retire it
I also wrote a petition in 2021 on Citizen.org that needs to be updated. Some of the top docs in the field, including a past president of the American Urological Association (AUA), signed it. You can still sign it.
The TR risk
According to the Mayo Clinic, the risk of sepsis with transrectal—some critics call them transfecal—biopsies is approximately one to two patients in 100 get potentially disabling and life-threatening sepsis. That's not peanuts since millions of men undergo prostate biopsies worldwide each year.
Researcher Truls Bjerklund Johansen has estimated, based on his figures from Norway, that about 2,000 American patients a year die from transrectal biopsies.
Many American urologists are skeptical. They insist TRs are safe in their hands. I have heard this over and over as urologists claim their biopsies are just fine.
Warning: What your urologists don’t know can be potentially hazardous to you.
Sepsis-transrectal biopsy links in most cases are never found. Patients die 30 days or even more following TR biopsies. Their urologists and patients’ families don’t make the connection.
This risk is hardly mentioned in the U.S., but was front-page news in Norway and helped start a biopsy reform movement in Europe, Australia, and elsewhere in the world led by Agnes Gulbrandsen, a hairdresser from Oslo, whose father died from a mysterious sepsis infection and by her father’s urologist, Bjerklund Johansen. Also, the TRexit group—a coalition of urologists from around the world—that has been working for a ban of transrectal procedures.
(Read about the Norwegian experience: https://www.medscape.com/viewarticle/989696 and Australia at https://howardwolinsky.medium.com/the-movement-to-make-transrectal-biopsies-go-extinct-e6e16538769f
Simple idea: Patients shouldn't die from sepsis caused by a transrectal biopsy
At the same time, something needed to be done to slow the march of antibiotic or antimicrobial resistance to which transrectal biopsies contributed as antibiotics have been dispensed in the U.S. like Pez to TR biopsy patients.
Ironically, some nervous urologists who have switched to TP biopsies still prescribe antibiotics to TP patients—a precaution that puzzles many urologists in Europe and even in the U.S. who find that TP makes antibiotics unnecessary.
What has your urologist told you?
(AI Creator Studio)
European urologists have been far more tuned in on the antimicrobial resistance problem, which results in infections difficult or impossible to treat potentially leading to severe illness, disability, and death. A hot mess.
In 2021, the European Association of Urology established guidelines making transperineal biopsies its preferred biopsy. Urologist Dr. Hendrick Van Poppel, policy chair of the EAU, told me that TR biopsies are tantamount to “medical malpractice” in Europe.
The EAU has emphasized stewardship of antibiotics and avoiding pushing needles “through the germy poo” as one urologist put it.
Progress has been slow in these United States. (Read story below about this.)
But there is a glimmer of hope coming later this month with the publication of an article by Jim Hu, MD, MPH, director of the LeFrak Center for Robotic Surgery at Weill Cornell Medicine/NewYork-Presbyterian Hospital and the Ronald Lynch Chair of Urologic Oncology at Weill Cornell Medical College.
(Dr. Jim C. Hu, Weill Cornell Medicine/NewYork-Presbyterian Hospital.)
Hu emailed me a teaser: “I do think the guidelines need to be revisited.”
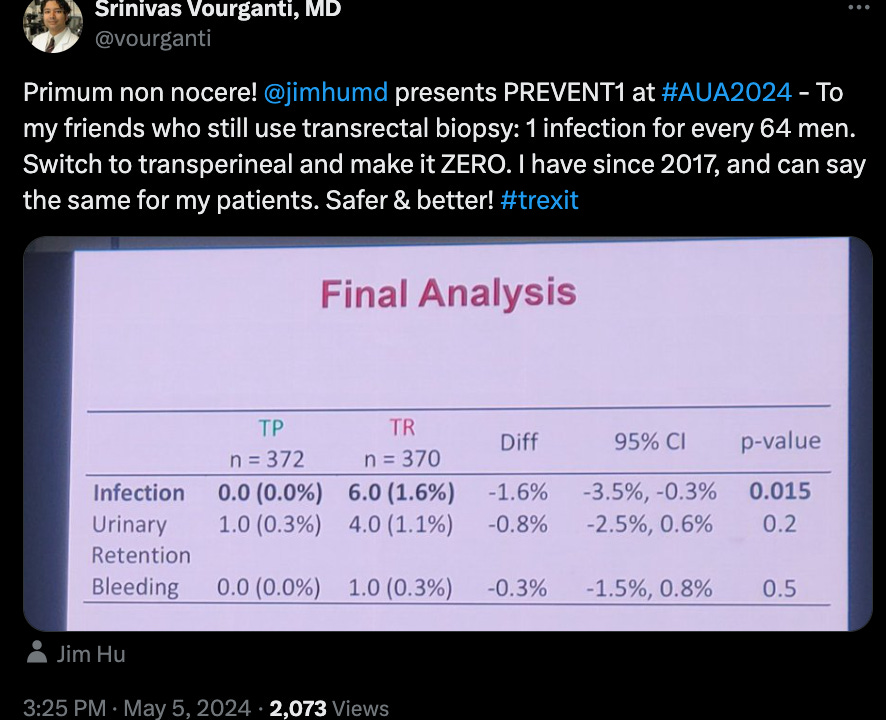
Hu shared some data in a session in May at the American Urological Association meeting:
(Data above from Dr. Jim Hu’s presentation at the AUA meeting. Note this doctor’s caption on the safety of TP.)
https://x.com/vourganti/status/1787217091906470199
Hu said he couldn’t comment in detail until the study is published, which should be this month.
Waiting for TP
I hope Hu’s right about his study potentially leading to change in the AUA guidelines.
I feel that we in the U.S. are living in an absurdist play, “Waiting For Godot,” in which the lead characters, Vladimir and Estragon, seem to exist only to wait for a mysterious character, Godot.
Godot never materializes, so the men’s existence seems absurd. They are trying to fulfill a purpose that can never be fulfilled.
We’re likeVladimir and Estragon waiting for the U.S. urology community and guideline writers to wake up and endorse TP biopsies.
Moving the biopsy needle to the TP (Part II)
By Howard Wolinsky
The biopsy needle has moved in Europe and Australia to transperineal procedures that avoid the rectum. There has been some movement toward TP in the United States, but it is slow.
I appeared recently on the GU Cast co-hosted by long-time TP proponent Declan Murphy, MD, director of Genitourinary (GU) Oncology, and Director of Robotic Surgery at the Peter MacCallum Cancer Centre, University of Melbourne. He also is one of the leaders in TRexit, an international group of urologists (with a penchant for punning) calling for the demise of transrectal biopsies.
(Dr. Declan Murphy, TR opponent.)
Murphy told me that 90%+ of prostate biopsies Down Under are performed transperineally. He says infections virtually disappear. (Nothing is 100%.)
Australian urologists are given an incentive through their health system to do TP biopsies. They get significantly higher fees to follow the transperineal rather than the transrectal road. Money talks.
There are similar rates in the United Kingdom and in Norway, where there was an overnight change because of the bad publicity fromTR shown to have killed a patient. (See Part I.)
The U.S. lags behind much of Europe in TP as it lags in use of MRIs as part of the diagnosis of prostate cancer and in Active Surveillance to avoid aggressive surgery and radiation therapy.
Hard to find in the U.S.
Meanwhile, transperineal procedures can be hard to find in the United States though availability is scaling up slowly. Sadly, we generally can’t find our ass from a hole in the ground in the Land of the Free and the Home of the Brave.
The national rate for transperineal biopsies in the U.S is roughly 10%, up from 5% two years ago, according to urologist Matthew Allaway, DO, founder of Perineologic, developer of an updated, less-invasive system of transperineal known as PrecisionPoint. Doubling sounds like a big deal. But the numbers are so small.
TP rates among the educated readers of TheActiveSurveillor.com are a far different story.
I found in a small survey that about one-third of respondents had had a transperineal biopsy while 49% said their next biopsy will be transperineal vs. 10% who said it would be a transrectal. The rest were unsure.
(Have an opinion on biopsies or digital rectal exams, why not respond to the anonymous TAS survey? Sound off here: https://forms.gle/QVXTXmuTrHjTppKq8 )
Obviously, respondents to TheActiveSurveillor.com Poll are not typical low-risk prostate cancer patients. I suspect they are better informed about their options and even are willing to travel to get a TP and feel comfortable questioning their urologists about their experience with TP vs. TR.
AUA and the debate
As a consumer reviewer, representing myself and also the AnCan Foundation, in the name of patient safety, I urged the American Urological Association in 2023 to prioritize transperineal biopsies in their new early detection guidelines.
I recommended they follow the lead of their counterparts at the European Association of Urology.
AUA was mainly focused on safety issues and demanded high-quality A-1 level randomized controlled trials—the champagne of research designs— before considering a major change to patient care.
In 2023, AUA did give the TP biopsy a small bump, making it an equal in safety to TR biopsies.
Hard to argue with the emphasis on obtaining the highest level of proof before making a major decision.
But some critics have suggested the AUA is dragging its heels to maintain the status quo and spare urologists from having to spend $40k to set up their practices for TP and also from spending the time to be trained in the new technique.
(Read about the differences between the biopsy approaches between AUA and EAU.)
More waiting?
I was told in 2023 that randomized clinical trials would come within a year. And indeed, they they have started to be published. Unfortunately, I think these studies have created a cloud of confusion with inconsistent results.
A single-center trial led by Badar Mian, MD, professor of surgery in the division of urology at Albany Medical College in New York, showed that TR and TP yielded similar results in terms of safety. Many criticized the study design, contending it was not big enough to find sepsis and relied on called-in complaints about infections, which they said were not representative of sepsis.
(Dr. Badar Mian of Albany Medical College in New York.)
Mian just published a study in the July edition of the Journal of Urology that challenged claims that TP finds more prostate cancer than TR. His group found no clinical significance in what a Journal editorial described as a “well-done clinical trial.”
The editorial states: “The authors are commended for their work, having contributed level I evidence that there is no difference between TP-Bx [transperineal biopsy] and TR-Bx [transrectal biopsy] in the detection of csPCa [clinically significant prostate cancer], infectious complications (2.7% vs 2.6%, respectively), and noninfectious complications (2.2% vs 1.7%).
So, to date, more or less, a tie between TR and TP.
What’s in the offing?
We’ll know soon whether Dr. Jim Hu’s study meets AUA Level-1 evidence standards, enough to warrant a change. (See Pari I.)
Hu had done an earlier study that came close to showing a statistically significant advantage to TP. The study was extended and more patients included to make it powerful enough to predict sepsis.
Meanwhile, the medical world isn’t exactly treating the TP vs. TR debate like a medical emergency even though patients lives and health are at stake. The doctors are taking their time—and being cautious—before releasing data and changing guidelines. That’s their nature, and is not necessarily a bad thing, unless you’re one of the five American patients who suffer death by biopsy each day per the Norwegian research.
As a patient and a patient advocate, I have a different view. I told the AUA early-detection panel in 2023 that in effect the house is on fire—that they should act now and no longer wait for Godot or delay calling in the fire brigade.
ASPI releases bite-sized video shorts based on the AS 101 series
By Howard Wolinsky
Bill Manning, new executive director of Active Surveillance Patients International, announced ASPI has now launched a series of 70 shorts from the Active Surveillance 101 series.
AS 101 was intended as an introduction to AS from PSA and genetic testing to Gleason scores, diet and exercise featuring such noteables as Drs. Laurence Klotz, Jonathan Epstein and Stacy Loeb.
The program was a joint project of the AS Coalition: ASPI, AnCan Foundation, the Walnut Foundation, Active Surveillance Nationwide Support Group in Canada, and TheActiveSurveillor.com
Kudos to Bill for creating the CliffsNotes to the AS 101 course: https://aspatients.org/shorts/
He also will feature a one-minute trailer at the ASPI table at the Prostate Cancer Research Institute this weekend, September 7-8 in Los Angeles.
Bill and I will be running a live-and-in-person support group at 12:15-1:15 p.m. Saturday, Sept. 7 at PCRI. On Sunday at 8 a.m., I am hosting Dr. Klotz in an “Ask the Expert” program. (Klotz is the expert—so bring your questions. Klotz is giving a keynote on Saturday.
Register for the first in-person PCRI meeting since COVID emerged in 2020.
Hope to see you there.
Caregiver vs. care partner survey
I am still trying to sort out whether to use caregiver vs. care partner to describe who we patients with chronic disease obtain support.
Can you weigh in at https://forms.gle/Ezv9cmTGMe9CG4VC8
PCF Canada holding webinar on whether Gleason 6 is a cancer
The Prostate Cancer Foundation Canada and its Active Surveillance Nationwide Support Group are observing Prostate Cancer Awareness Month with a program on whether Gleason 6 lesions should even be considered a cancer at all.
Dr, Alejandro Berlin, a researcher and radiation oncologist at Princess Margaret Cancer Center in Toronto, will be the featured speaker at 7:30 pm Eastern on Thursday, Sept. 12. Register here: http://bit.ly/PCAM24-AS
Ale and I are members of the Gang of Six (on Gleason 6) that has been calling for renaming Gleason 6 as a non-cancer. We coauthored Low-Grade Prostate Cancer: Time to Stop Calling it Cancer, the most-read article in the Journal of Clinical Oncology in 2022. It sparked controversy—and more papers.
Our group just embarked on a new study oversampling for Black men and Latinos, who often are missing from research on prostate cancer, especially on Active Surveillance.
Register for the webinar here.