UCSF's Dr. Matt Cooperberg: Why some prostate cancers shouldn’t be called ‘cancer’
Also, check out the ASPI session on clinical trials and YOU- r. Geo, and more.
(Editor’s note: I ran across this Q&A by University of California San Francisco medical writer Elizabeth Fernandez about Grade Group 1/Gleason 6 and why it should be renamed a noncancer. I am reprinting her piece with permission and linking back to the original. Matthew Cooperberg, MD, MPH, of UCSF, is the featured expert.
( Disclosure: I have been working with Dr. Cooperberg on a campaign to redefine Gleason 6 (Grade Group 1) as a non cancer. See. Experts are divided on this topic.
By Elizabeth Fernandez
Men could benefit from fewer unnecessary treatments and reduced anxiety if their doctors stopped calling certain changes in the prostate “cancer,” according to prominent UC San Francisco prostate cancer expert Matthew Cooperberg, MD, MPH. In fact, the changes are a low-grade, extremely common condition among older men that won’t metastasize or kill, but should be actively monitored, he says.
Featured Expert
Matthew Cooperberg, MD, MPH
Professor, Urology
Cooperberg, who has won awards for his contributions to the field, helped launch a national registry for patients with prostate cancer and other urologic diseases. He is a prostate cancer specialist and surgeon, and part of the urologic oncology team at the UCSF Helen Diller Family Comprehensive Cancer Center.
He explains the reasoning behind the change and the importance of monitoring low-grade disease.
Prostate cancer is the second leading cause of cancer deaths among men in the U.S., but you and other national experts believe that some instances should not be classified as cancer at all. Why?
That’s right. Low-grade prostate cancer, called grade group 1, or GG1, never spreads or kills. But GG1 isn’t normal and should be actively monitored. GG1 can co-exist with or evolve into “real” prostate cancer, but patients with pure GG1 should not be burdened with a cancer diagnosis that has zero capacity to harm them.
How could patients benefit?
There are a host of social, psychological and financial implications. Patients would benefit from less stress and anxiety, and excessive treatment rates would drop. Also, hopefully, they would no longer be denied or overcharged for life and health insurance policies. This would all lead to a public health improvement.
What should early-stage prostate cancer be called instead?
There have been multiple alternatives proposed over the years. The alternative that seems to have the most traction among clinicians and pathologists is “acinar neoplasm,” which describes GG1 as an abnormal growth visible under the microscope, but not one with the potential to spread or kill.
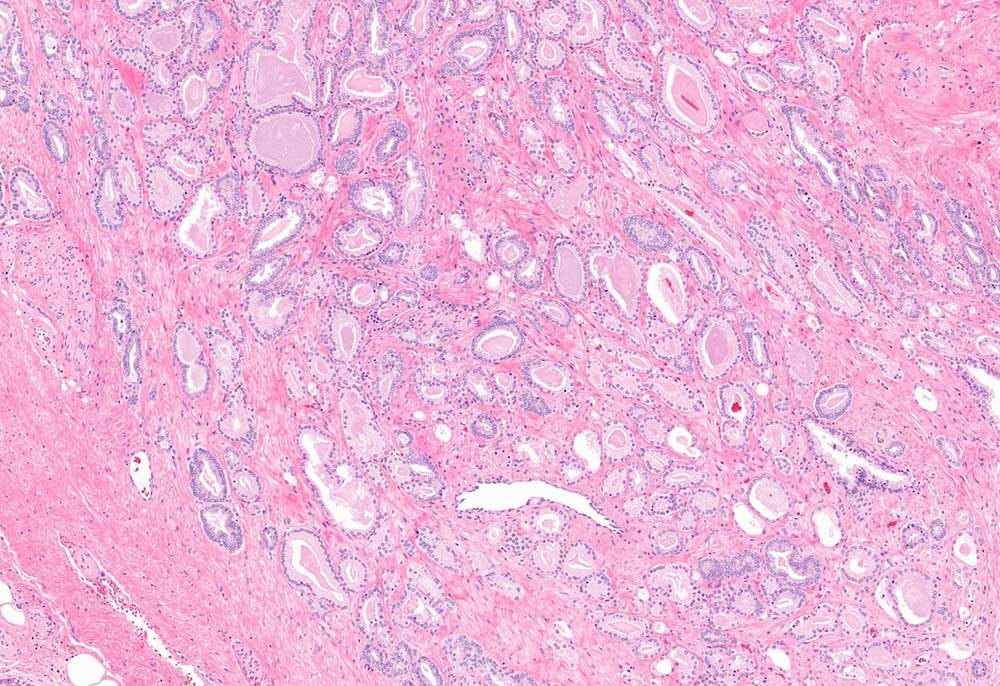
This is low grade (GG1) prostate cancer – this cancer has low risk of metastasizing.
This is high grade (GG4) carcinoma which has spread to soft tissue.
Images by UCSF
Would some patients still prefer aggressive treatment by thinking they are “doing something?”
This phenomenon – treatment without strong clinical indication, based on anxiety – definitely does happen but is becoming less common, and, principally, represents a failure of counseling. It is our job to help patients understand that low-risk prostate cancers often do not progress. If they do, it’s usually slowly, over many years and, in most cases, can be picked up by active monitoring well within the window of opportunity for cure.
Do you have any worries about changing the name?
A subset of GG1s will progress over time to potentially lethal cancer, so active monitoring with blood tests, imaging and biopsies is essential. One concern is that patients may not take seriously the need to monitor the progression of the condition if their doctor doesn’t use the word “cancer” in explaining the diagnosis. But this is only a theoretical concern, and colleagues and I were recently awarded a grant from the Centers for Disease Control and Prevention (CDC) specifically to address this concern with diverse patients across California.
Has active monitoring made strides in recent years?
A dozen years ago, active monitoring was still largely an academic enterprise, used in only 10% to 20% of low-risk cases; the rest were treated immediately. Today active monitoring is endorsed as the preferred management for low-risk prostate cancer by all major guidelines, and monitoring rates have risen past 60%. This figure is still too low, but we’re making rapid progress. We are also starting to personalize active monitoring protocols, tailoring intensity based on clinical criteria and are avoiding repeat biopsies in particular when safe to do so. However, there is still major variation in the adoption of monitoring crossing urology practices and individual urologists.
How far have we come in understanding prostate cancer?
We used the word “cancer” literally for millennia to describe a disease characterized by inexorable spread and lethality. In the modern era, the term describes a huge spectrum of abnormal growth patterns among cells in different parts of the body. Some are rapidly lethal, and others completely indolent, and this huge heterogeneity exists within the spectrum of prostate cancers as well. We’ve made huge progress in understanding prostate cancer’s typical progression in people. We’ve grown quite accurate in being able to determine when it is aggressive and when not, and can improve this accuracy even more with emerging genomic and other tests.
Elizabeth Fernandez, senior public information representative at UCSF, covers the clinical cancer program, women’s health, tobacco, emergency medicine, radiology, urology, and dermatology. Previously, she was a journalist for more than two decades, covering investigative stories, health, social justice, law enforcement and education at newspapers around California. She holds degrees from Santa Clara University (BA, English) and Columbia University Graduate School of Journalism (MS, Science).
How you can help in clinical research on Active Surveillance
By Howard Wolinsky
Without clinical trials, such as ProtecT, patients with lower-risk prostate cancer would have had no choice other than aggressive treatment with risks of side effects impacting their quality of life. I have participated in about a dozen trials as a patient and a patient researcher.
I highly recommend participation in trials. I have been in studies on diet and low-risk prostate cancer, genetics and medications and low-dose aspirin and preventing heart attacks.
Look for trials on Active Surveillance that you potentially can join at ClinicalTrials.gov
Active Surveillance Patients International (ASPI) is holding a webinar at 12:00PM ET Saturday, November 30, entitled “How you can help in clinical research on Active Surveillance.”
REGISTER HERE: https://zoom.us/meeting/register/tJIocOCupz4jGtX8fHJ036bYGHYIjLfwfRzk
Speakers will include Kevin Shee, MD, PhD, a researcher at the University of California, San Francisco, and Mike Scott, founder of Prostate Cancer International and an early advocate for Active Surveillance.
Dr. Shee has been involved in multiple studies, the most recently one on whether men 75 and above should stop active surveillance.
Though not a prostate cancer patient himself, Mike Scott was the founder of one of the first support groups for men on AS. ASPI this year presented him with its 2024 Thráinn Thorvaldsson Award for Patient Advocacy.
A question-and-answer session will follow the presentations.
If you have questions, please send them to: contactus@aspatients.org
Climbing Dr. Geo’s ‘Prostate Cancer Summit,’ addressing AS, herbs, diet, prostate massage, and more
By Howard Wolinsky
Dr. Geo Espinosa (you may know him as the author and podcaster “Dr. Geo,”), the naturopath specializing in prostate care on faculty at New York University, is hosting a free week-long “Prostate Cancer Summit” you shouldn’t miss.
The free event runs November 19 - 25, with an “encore weekend” November 29 - December 1, 2024. Register here: https://drtalks.com/summit/prostate-cancer-summit/?uid=814&oid=83&ref=4266
(Dr. Geo)
Geo interviewed about 40 experts on prostate cancer—plus me. The interviews cover a full range of prostate cancer topics.
Speakers include urologist Dr. Stacy Loeb of NYU, on lifestyle; Dr. Sanoj Punnen of the University of Miami, on the value of MRI and biomarkers in diagnosing prostate cancer; Man Up podcaster Justin Dubin, MD, on regaining sexual health after treatment; Donald Abrams, MD, on marijuana’s role in prostate cancer management; and Eric Yarnell, ND, on herbs and PCa.
Geo interviewed me about Active Surveillance.
Register here: https://drtalks.com/summit/prostate-cancer-summit/?uid=814&oid=83&ref=4266
Find me here. Who else do you know?
Share your experience with shared decision making
Europa Uomo, a major European federation of national patient prostate organizations, does some of the best research on PCa and its impact on patients. Europa Uomo has just launched its latest survey on shared decision making,
Why not share your opinions, here: europa-uomo.org/eu-press ? The survey is anonymous and takes about 25 minutes to complete.