Biopsies: Going, going but not totally gone
What's the frequency, Laurence? Five years for biopsies is now the default.
By Howard Wolinsky
Twelve years ago, when I started riding the active surveillance train, I began having a transrectal biopsy on an annual basis for several years. I had five biopsies between 2010 and 2013.
We react to prostate biopsies in our own way. I didn’t find them horribly painful though I know some men do--not that I loved the experience.
I just put up with biopsy needles, just as I do the dental drill.
A little lidocaine can go a long way, right? In prostate biopsies and dental fillings.
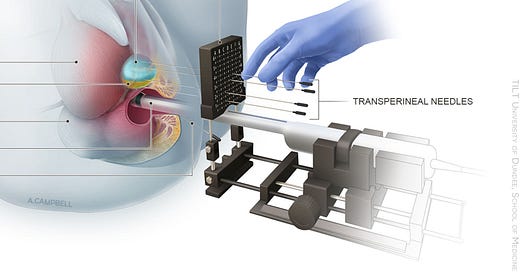
(Transperineal biopsy)
I never have an infection, maybe because I got high doses of powerful antibiotics. Or maybe I was just lucky.
The annual biopsy ritual was a precaution taken in the protocol for active surveillance (AS) at Johns Hopkins, a pioneer in AS. My urologist at the University of Chicago followed that protocol.
Turns out there is a joke among urologists about the annual biopsy. (Not that it’s all that funny from my POV.)
Laurence Klotz, MD, the father of AS and Chair of Prostate Cancer Research, Sunnybrook Health Sciences Centre, at the University of Toronto, retold the quip on September 10 at the annual patient conference online of the Prostate Cancer Research Institute. (Guide to Klotz session.)
To paraphrase: Surgeons joked that if they did annual biopsies for 15 years, they were performing in effect radical prostatectomies one needle biopsy at a time.
Not really true, but it’s only a lame joke.
I once asked Jonathan Epstein, MD, Hopkins’ guru of Gleasons and prostate biopsies, a question along the lines of how many angels dance on the head of a pin.
But instead, it was: How many biopsy cores would it take to in effect perform a prostatectomy?
He didn’t miss a beat: 10,000. (Talk about an ultra-saturation biopsy.)
In my case, because the biopsies after the diagnosis were coming up empty year after year and my PSA was stable, I went on a “biopsy vacation.”
I switched urologists in 2016. My new doctor wanted a “baseline.” That year I had my last biopsy to date. Maybe my last forever.
My new doctor, Brian Helfand, of NorthShore University Health System outside Chicago, at that point, recommended biopsies every two years. So, in this scheme, I would bw due for a biopsy in 2018.
I told him that a two-year interval, not stand, that I, like many other patients, would go on strike or rebel. Biopsies, even every two years, seemed excessive.
I pointed to the PRECISION trial, published in the New England Journal in 2018: “A total of 500 men underwent randomization. In the MRI-targeted biopsy group, 71 of 252 men (28%) had MRI results that were not suggestive of prostate cancer, so they did not undergo biopsy.”
In Britain that year, guidelines were released calling for MRIs before biopies: “Men with suspected prostate cancer should be offered multi-parametric magnetic resonance imaging (mpMRI) to reduce the number of invasive and unnecessary biopsies, says draft guidance from the UK National Institute for Health and Care Excellence. The technology produces a detailed image of the prostate that helps clinicians decide whether a biopsy or subsequent treatment is needed.”
(Funny enough, Scott Eggner, MD, from the University of Chicago, who put me on AS and annual biopsies, was a co-author of the PRECISION study.)
In 2018, when I mentioned reducing the frequency of biopsies for my very low-risk prostate cancer, Dr. Helfand, really a good guy, basically said, “Tough.”
He asserted biopsies were the best tool in his toolbox, the “gold standard.”
I think he has softened his position since then. I’ll explain why in a moment.
Meanwhile, Klotz said at PCRI annual biopsies “clearly were too much.”
He and other leading lights told me years ago I ought to stop undergoing biopsies--unless my PSAs started rising. My PSA (prostate-specific antigen) scores, if anything, have trended down from a high of 9 to 4.5 and have remained stable.
I was prepared to go to St. Louis or Cleveland to get a micro-ultrasound, an alternative or a supplement to MRIs, if my PSA blood level rose. I preferred those options to undergoing another biopsy—especially a transrectal, which carries a risk for sepsis, but also a transperineal. I was biopsied out and ready to stand my ground.
It never came to that.
Last year, Helfand told me he was going to monitor my PSA. If my PSA rose a lot, then he would order an MRI, which is emerging as the initial go-to test following a rising PSA. Biopsies generally are the next step if MRIs spot troublesome lesions.
I was in the first cohort to undergo MRIs for prostate in the early 20-teens. Back then--in olden times--it was biopsy first and then MRIs. Now it’s becoming the rule that MRIs come first if PSA is rising, then, if needed, a biopsy.
In 2020, my 10th anniversary on AS, Eggener said he was glad he had spared me from surgery but wished he could have saved me from all the biopsies. Me, too.
Still, biopsies have not gone away and won’t for some time.
In his practice, Klotz said in the past he had switched to biopsies every three years ago. Now biopsies are less frequent, maybe four to five years.
“Patients don’t like it (biopsies), first of all. That’s part of the driver. … MRI alone could not find progression [of prostate cancer] reliably but if that progression is mainly 3+4 [Gleason Grade Group 2] does it really matter if you find it this year or can you wait another year or two to find it?
“I want to be very clear. We’re not ready to stop doing biopsies, but as time goes by, I think everyone in this field is doing them less and less frequently.”
Klotz, who has moved exclusively to transperineal biopsies to keep patients safe from sepsis, said, “Now, my default is if I see everything is fine, and it’s been five years since his last biopsy, I say, okay, it’s time.”
Answer the survey
Active Surveillance Patients International, AnCan Virtual Support Group for Active Surveillance, Prostate Cancer Support Canada, and The Active Surveillor newsletter are asking you to participate in a survey on patient attitudes toward Active Surveillance,
To participate in the survey, click here: https://www.surveymonkey.com/r/W69XXDS
The survey is open to patients on AS for low-risk Gleason 6 prostate cancer to favorable intermediate-risk prostate cancer as well as those who have moved on to treatment,
Data will be used to inform policymakers, guideline writers, and clinicians about where we stand on key issues.
For example: Will renaming Gleason 6 lesions as noncancerous reduce mental distress and financial toxicity in patients on AS? Should U.S. guideline writers, as their European counterparts did last year? favor safer transperineal biopsies vs. transrectal biopsies that can cause sepsis and other infections?
Moving AS to the next level
By Howard Wolinsky
The Active Surveillance Coalition, a collaboration of leading support groups for active surveillance (AS) for prostate cancer, is sponsoring a webinar at 9 a.m. Vancouver/12 p.m. New York/5 p.m. London/6 p.m. Amsterdam on Thursday, Nov. 17 to discuss how we can move the needle on AS, close monitoring of prostate cancer.
AS leaders from Sweden, Holland, the United Kingdom, and the state of Michigan’s will share their “secret sauce” for reaching AS rates of near 90% and above.
The free webinar is entitled “Moving AS to the next level: Can we help more patients?”
Register here: https://bit.ly/ASnextlevel
The United States has lagged behind other wealthy countries in AS acceptance though the approach started here and in Canada in the late 1990s. AS uptake with AS finally reached a majority of 60% in 2021. The American Urological Association in 2022 set a new goal of 80% In 2010, only 6% of patients qualified for AS opted for this approach.
Several European countries and the state of Michigan’s MUSIC (Michigan Urological Surgery Improvement Collaborative) program have reached AS uptakes of around 90% or higher.
Panel members will present their stories followed by a discussion and a Q&A involving the audience.
Sign my petition to phase out transrectal biopsies. Read why: https://chng.it/7bQsWSfK Once we hit 1,000 signatures, we should begin letting Congress, Medicare, and the American Urological Association know. Please make no donations. This effort requires your signatures, not your money—at this point.



It would be too good to be real if someday the biopsy was obsolete, but given the ever present reliance on PSA by many urologists I expect it may sometime before we no longer have to contend with the prospect of repeated biopsies.
Richard, We're stuck with them for now. But maybe the next generation will get a break. Or at least transperineal will be more widely available. AUA needs to change its policies on TP vs. transrectal, too. This process has begun.