EXCLUSIVE! Read all about it: 'Deep Prostate' spills the beans on why AUA has no guideline for screening PCa patients for emotional distress
Part 3 in a series on mental distress and prostate cancer.
By Howard Wolinsky
I didn’t meet “Deep Prostate” (a.k.a DP) in a shadowy parking garage as Bob Woodard encountered “Deep Throat,” his secret FBI leaker on the Watergate scandal in the ‘70s.
I encountered this leading urologic oncologist while on the beat—as far as I know—as probably the only two-time Pulitzer Prize-nominated reporter on the planet who specializes in covering AS and low-risk prostate cancer.
(Washington Post reporter Bob Woodward played by Robert Redford in “All the President’s Men.”)
Readers of TheActiveSurveillor.com know that I consider emotional distress as one of the major overlooked issues confronting patients on Active Surveillance (AS) for low-risk Gleason 6 prostate "cancer.”
I was just getting to know DP, when I asked about emotional distress (anxiety, depression, stress, fear, anger) and prostate cancer. DP turned out to be involved with setting guidelines for AUA.
I asked DP why AUA guidelines groups have not taken seriously the issue of emotional distress, not only in AS patients but in those awaiting or having undergone radical prostatectomies.
I am sharing insider thinking on this subject. I asked for permission to quote DP by name but never received a response. I likely didn’t hear back because this candid interview is somewhat shocking—to me at least.
DP acknowledged that emotional distress is not uncommon among prostate cancer patients on AS. But the urologist said AUA guideline writers don’t feel there’s sufficient scientific proof to warrant a guideline.
Anxiety and prostate cancer are as common as prostate cancer itself as the second most common cancer in men. Simple as that, DP said.
“People who have tumors or have masses who we're watching have anxiety, a lot of people A lot who have cancers and are doing follow-ups get scanxiety [anxiety over MRIs and other tests]. Two, three days, before that test can bring up a fair amount of anxiety for people. I wouldn't say it's ubiquitous. There are some people who don't experience that. But it's very, very, very common.
“The way I always talk to people about this is, first of all, to recognize that this is natural. This is normal, so embrace those feelings and those emotions. The sooner you embrace them and understand them, the sooner you can move through them. But if you keep pushing them off, you're just kind of delaying the inevitable, and you're making yourself kind of suffer through them.
“Understand that you're having emotions and whether it's anxiety, anger, fear, whatever it may be, call them out, name them. You don't have to say it out loud but kind of understand what you're going through. Recognize that there's a physiology associated with emotion, but that physiology doesn't need to last forever. We make the emotion last longer. Once again, whether it's anxiety, fear, or anger, we make it last longer. And once you recognize that it's just a normal process then it becomes easier to manage. It doesn't necessarily make it go away, but it makes it easier to understand and manage.”
DP does not routinely screen patients for emotional distress, except testicular cancer patients. “There is specific data that says they are kind of a unique population diagnosed at a young age, and there are higher rates of anxiety and depression, and mental health disorders in the testicular cancer group. And there are higher rates of suicide. And actually, if you look at the overall population-based numbers, more testicular cancer survivors die of suicide than of testicular cancer.
“There's no data in prostate cancer,” DP claims. There's very little data in those groups. NCCN [National Comprehensive Cancer Network], the other major guideline-writing group for prostate cancer, recommends screening all cancer patients for emotional distress. The American Cancer Society, the American Society for Clinical Oncology and the American College of Surgeons also recommend screening of all cancer patients for emotional distress.
[Check my article on the elephant in the room: https://www.medscape.com/s/viewarticle/983434?src=#vp_2]
DP said, “All those other groups say they are evidence-based but they don't they don't base their guideline work necessarily on a systematic or evidence-based review.
“The AUA really only crafts guidelines and guidelines statements around evidence and where evidence exists. People ask me: Why didn't the AUA say this or that? Or why didn't they do that? In the case of guidelines for emotional distress, the reason is there's no data. If you think it's an important question -- the polite response is always, you think it's a really important question, let's get the data. Let's write about it, and we'd be happy to support to support it.”
[Patient advocates, to the contrary, argue there is plenty of data showing the emotional impact of a prostate cancer diagnosis on the emotional health of patients, including suicides from depression brought on by the diagnosis and treatment of PCa.]
Earlier this year, an AUA spokesman told me the organization would be discussing the possibility of guidelines for screening for emotional distress in patients with prostate cancer. But it was a non-starter, as far as AUA guidelines writers, as Deep Prostate explained.
In October, an AUA spokesperson said: “The AUA agrees that emotional well-being is an important consideration for all patients with cancer, and we will continue to discuss the idea within each of our disease-specific guidelines.” That’s just lip service.
AUA and its sister organizations, the Society for Urologic Oncology and the American Society for Radiation Oncology (ASTRO), who often write guidelines together, need, as my old Chicago Sun-Times colleague, the late Eppie Lederer (advice columnist “Ann Landers”) would say, it’s time for AUA and others to “wake up and smell the coffee.” It’s past time for these ostriches to excavate their heads, take this problem seriously, and act in the interest of patients and doctors alike.
MSK urology chief and former AUA guideline writer supports guidelines for screening for emotional distress
By Howard Wolinsky
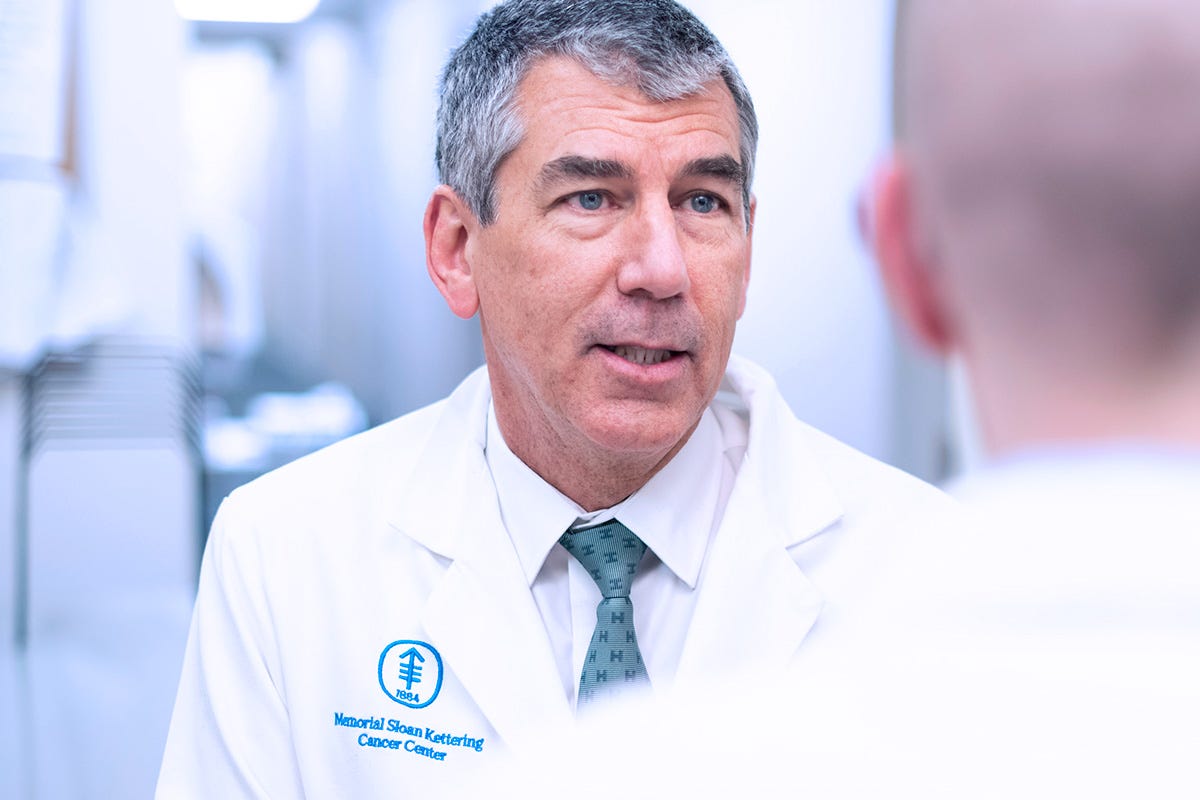
Dr. James Eastham, urology chief at Memorial Sloan Kettering (MSK) Cancer Center in New York, who chaired the American Urology Association committee that developed clinically localized prostate cancer guidelines, in collaboration with ASTRO, predicted in an interview in an interview with TheActiveSurveillor.com that AUA will eventually adopt mental distress guidelines.
He agreed that emotional distress is not uncommon in patients with low- or high-risk cancers, untreated or treated.
“Most of the year they're fine, but when it comes up for their semiannual-ish PSA check for the week or two beforehand, they start to get nervous. Anxiety is not unique to the surveillance population. It's unique to the cancer population and probably beyond that as well.
Unfortunately, he said emotional distress in prostate cancer patients historically was something that was “pushed down. [Patients were told:] Deal with it yourself. Pull yourself up by your bootstraps. Why are you so sad? Those types of things.” But he said he feels his colleagues increasingly are aware of these issues and are talking to patients about them.
Eastham is different. He works in an institution that is very supportive of screening and supporting cancer patients for emotional distress—several of the survey instruments for emotional distress were developed there. Retired MSK psycho-oncology pioneer Andy Roth, MD, who devoted his career to helping men with prostate cancer and their partners, developed emotional distress thermometers recommended by guideline writers at the National Comprehensive Cancer Network.
Eastham said patients need to be helped to better understand PSA testing. He said patients should “take a deep breath” and their doctors need to explain “what PSAs are and what they aren't.”
Scanxiety is common. But the biggest problem may be PSA Anxiety. We worry a lot about our PSAs. Our moods ride a roller coaster of ups and downs with even small blips in PSAs.
Eastham shared his view on PSAs: “Many people think that if their PSA goes from 4.1 to 4.2, their cancer's exploding. They don't understand that PSA is not a cancer marker; it's an indication of something going on in the prostate. And when you simplify only say, that there are other things that can impact your PSA test, so we shouldn't get too excited when they jump up and too happy when they go down.
“It's more a factor of trends over time. And it's not one test to one test. As these things don't change that quickly. It's an indicator, but it's not an absolute, oh my goodness, my PSA went from four to 4.3, now I need to be treated. And it's the conversation [urologists need to ]have with the patient. I think that that can go a long way to allaying some of that anxiety.”
(James Eastham, MD, urology chief at MSK Cancer Center.)
So chill guys. Another urologist told me many patients are very freaked out if their PSA hits 10 or above. This researcher and clinician said he doesn’t worry about PSAs until they hit 15 or above—and that PSAs any way are simply one factor to consider.
Eastham added: “PSAs are a marker of something going on in the prostate, but I don't think it should be under-interpreted, certainly, but I don't think one should over-interpret and use PSAs to make big treatment, decisions meaning surgery, radiation, focal ablation, those types of things, treatment decisions solely based on a PSA test.”
Eastham said he expects AUA, SUO, and ASTRO guideline writers to eventually join other organizations and guidelines for screening for emotional distress in patients with prostate cancer, whatever their grade,
He said, “I think it's very reasonable. The whole field [of prostate cancer care] has evolved, but it's taken decades. PSA became clinically utilized in the mid-to-late-80s. At that point, every man with a little bit of a blip in his PSA got a biopsy immediately, and every speck of Gleason score 6 was treated, whether it was surgery or radiation therapy. And we've appropriately evolved.”
Enter Active Surveillance. Many of us now following AS have encountered anxious (or greedy) urologists who tell us we’re ticking time bombs—even if only have one core with a microscopic speck of Gleason 6.
Eastham observed: “Some would say we've taken too long, and I would be in that camp as well, but I think that we evolved over time. And these mental health concerns: anxiety, depression, those types of things, I think are becoming more apparent to urologists. I think if you would have given a (emotional distress thermometer) questionnaire to men 20 years ago, most of them would have crumpled it up and thrown it in the trash. Not because the man didn't have any form of anxiety or concern, but because he was not comfortable sharing it.
“I think it's because it's become more accepted, and this is a long-winded answer of saying, yes, I think we should advocate for such screenings. It's because again, it's an evolution I think. We're becoming more comfortable realizing that there are these issues. And there are very good strategies to manage these issues even if it's like what you've done, have a [support] group. Have a [peer] group of like-diagnosed or like-minded men, and that might be a good way on a community level to handle some of these issues.”
Amen, Brother Eastham.
Previous articles in the series:
—European view of emotional distress:
European quality of life study: Anxiety and the uncertainties of Active Surveillance
(By Howard Wolinsky A large European study shows that even Active Surveillance patients with low Gleason 6 scores facing an extremely low risk of dying from prostate cancer, are grappling with emotional distress (anxiety/depression/stress). “Active surveillance seems to be associated with higher levels of depression or anxiety than treatments such as rad…
MUSIC addresses Anxious Surveillance
By Howard Wolinsky Anxiety is so common in men on Active Surveillance (AS) for lower-risk prostate cancer that we have a name for it: Anxious Surveillance. It’s common: 55% of us experience it. 10% experience severe anxiety that can drive us to seek aggressive treatment, according to a survey of 450 men who are on or were on AS.
C’mon. Why wait? Sign up for the ZERO AS support group in March
By Howard Wolinsky
For the past three years, I have run a special Active Surveillance support group for ZERO. Last year, our virtual support meeting drew 60 patients to talk about AS. It was by far the biggest session of any at the annual ZERO Summit.
Why not plan ahead and sign up for the program at 11 a.m. Eastern March 12, 2024.
Register in advance for this meeting:
https://us02web.zoom.us/meeting/register/tZUsfuqgrjIoG9AWf7voMhzT_UjdqbQQbQPA






Phemepark.
No one says emotional distress is unique to ASl et alone even to prostate cancer.
Maybe you're a new reader?
This newsletter and several support organizations, including AnCan and ASPI, have been trying to get leading organizations such as the American Urological Association to take anxiety and emotional distress issues seriously,
The American Society for Clinical Oncology, the American Cancer Society, the American College of Surgeons and the National Comprehensive Cancer Network all urge that ALL patients with cancer be screened for emotional distress. The AUA and ASTRO do not make this recommendation.
Here's some background: https://open.substack.com/pub/howardwolinsky/p/deep-prostate-spills-the-beans-on?r=4ah4&utm_campaign=post&utm_medium=web
The focus here is on Active Surveillance, long the Rodney Dangerfield of cancers. We're not in a pissing match with other prostate cancer patients over who has it worse.
The issues are similar but different for the spectrum of patients. The issues are different for individual patients. There are many patients with low-risk prostate cancer who easily could go on AS but instead decide they MUST have surgery and take on the lifestyle risks.
That's their call and that of their doctors--some doctors won't operate on these men because they consider it unethgical to perform surgery on healthy patients.
A leading Italian psychologist says, "Prostatectomies don't cure anxiety."
HW
Thanks, Richard.
Though the comments were very interesting. from the AUA person.
Howard