Look mom--no gadolinium. And no more claustrophobia? New approaches coming to improve Active Surveillance experience
Developing: New research shows fewer men with Grade Group 1 are undergoing radical prostatectomies
By Howard Wolinsky
A new generation of urologists is revolutionizing prostate cancer care, bringing innovative approaches to improve the experience of Active Surveillance (AS) patients with low-risk prostate cancer. These advancements in prostate cancer management promise better patient outcomes and enhanced quality of life.
How about eliminating gadolinium contrast and its risks for crossing the blood-brain barrier? Or reducing time in the MRI scanner to alleviate panic attacks, anxiety, and claustrophobia in prostate MRI procedures? These breakthroughs are transforming urologic care for men on Active Surveillance protocols.
Get a taste here: Benjamin Pockros, MD, a third-year resident at the University of Michigan (Go Blue!) School of Medicine, has never performed a transrectal biopsy, only a transperineal biopsy. Why? Transrectal biopsies carry risks of infection and sepsis, reportedly causing 2,000 deaths annually in the U.S., making transperineal prostate biopsy a safer alternative in urologic oncology.
(Dr. Benjamin Pockros)
Pockros said he and his colleagues expect to rely more on MRIs for prostate cancer than urologists have in the past to enhance the patient experience for men on AS, who may face multiple prostate MRI scans over their Active Surveillance duration.
“Prostate MRIs have been really helpful, but there are also unfortunate drawbacks for patients. Traditionally, it can take an hour. It's hard if you're claustrophobic. You have to get an IV for contrast from a nurse. Contrast agents go into your body, and it can be an expensive scan as well. [It costs about $1,000 for the contrast agent and up to $3,000 for a prostate MRI scan.]
“And so, for men on Active Surveillance who may undergo multiple prostate MRIs in their lifetime, it's really challenging. And the concern could be if it's an uncomfortable experience or costly procedure, it may deter men from adhering to Active Surveillance protocols, which defeats the purpose of prostate cancer surveillance.”
Claustrophobia, needle phobia, and fear of contrast agents can deter men from pursuing AS for prostate cancer.
The University of Michigan [Go, Blue!] has started to explore offering prostate MRI without contrast for men on Active Surveillance, a significant step in non-invasive prostate cancer monitoring.
“At least at the University of Michigan, we've primarily only performed transperineal biopsies for AS patients. We'll do transrectal for very unique circumstances, but all of our residents know how to do transperineal biopsy, but we just don't really teach or frequently do transrectal,” he said.
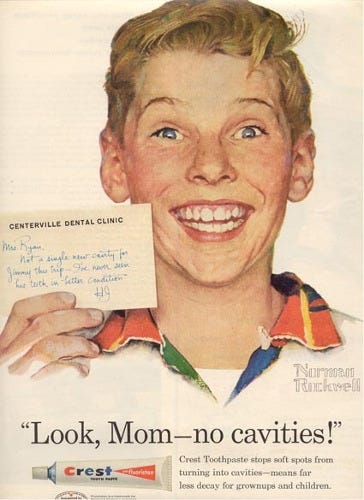
(You old-timers should remember this ad for Crest from the late 1950s. Maybe we can update with ads o saying ‘Look, Mom—no gadolinium?)
Pockros and his colleagues are taking another step regarding MRIs. They have conducted research on prostate imaging, demonstrating the advantages of biparametric MRI vs. multiparametric MRI in prostate cancer detection.
Biparametric MRI? You probably have never heard of the biparametric approach to MRIs, which uses only two factors in making prostate scans that will have a dramatic impact on prostate cancer diagnostics.
Pockros explained: “A multiparametric MRI traditionally has three phases: one that focuses on anatomy called T2-weighted imaging, one that focuses on the cellularity of the cancer cells called DWI (diffusion-weighted imaging), and then a contrast component called dynamic contrast enhancement. Getting rid of the contrast agent changes the name from multiparametric MRI to biparametric MRI.”
Researchers reported that of all bpMRIs, 96% were reported to have adequate evaluations by radiologists—effectively demonstrating the feasibility of adopting this innovative imaging technique at the University of Michigan for prostate cancer screening.
Antonio Westphalen, MD, Section Chief of Abdominal Imaging at the University of Washington and UW professor of radiology, said, “In men undergoing Active Surveillance for prostate cancer, the goal of MRI is to monitor for changes over time, such as new lesions or growing lesions, rather than to reassign a PI-RADS score. These changes are best detected with T2-weighted and diffusion-weighted imaging, making biparametric MRI — which omits dynamic contrast — a good option for prostate cancer monitoring.
“It shortens scan time, improves patient comfort, lowers healthcare costs, and retains the key sequences needed for effective prostate surveillance. Successful implementation, however, requires careful coordination: scheduling systems must accurately identify patients on surveillance to avoid unnecessary full protocols, and ensure that men needing full multiparametric MRI — such as those with diagnostic uncertainty or hip replacements — are correctly routed.”
Pockros, who presented his research paper Monday at the American Urological Association annual meeting in Las Vegas, ticked off the many ways biparametric MRIs can help patients:
--Biparametric MRI is simpler than multiparametric and makes scanning a speedier process that may improve the patient experience for men.
It can reduce tube time to about 15 minutes from one hour. Reduced MRI scan time can lower anxiety and claustrophobia in prostate imaging. It may also improve access to care for patients by increasing the number of daily MRI slots available with saved time.
I get claustrophobia in the MRI tube and have had to white knuckle it through. I have had a tech torture me, like Torquemada the Tech at UChicago during a prostate MRI in 2011. [On the other hand, I had MRIs where a tech gently talked me through a shoulder MRI with my face covered. I also took a dose of diazepam, the Actine Surveillor’s Little Helper.]
--Patients skip the IV stick to deliver contrast. “Now, you don't need to get an IV for MRI. Now, you don't need to go through all the screening surveys to see if you're safe for contrast agents. Now, you don't need to experience the potential risks of gadolinium. There's some research that it can deposit in areas of your brain. That's still being discovered. And there's also research that shows that doing it without contrast is hundreds of dollars cheaper,” Pockros said.
--No gadolinium, the contrast agent. Pockros said that evidence is strong that most men don’t need gadolinium to get decent prostate images to identify clinically significant prostate cancer. This comes from a large clinical trial in Europe, called “PRIME,” which compared diagnostic accuracy with and without contrast.
There have been concerns about whether gadolinium is a risk for patients because the residues of the metal can potentially deposit in the brain, bones, and vital organs. Radiologists generally say they have lowered doses, but the Michigan researchers said they can just avoid gadolinium in most patients on Active Surveillance.
[Check out my story on gad in MedPage Today. Also I won a “Chicago Pulitzer Prize,” the Lisagor, from the Chicago Headline Club for this expose: https://ziniy.com/chicago-medicine-magazine/preview/october-2019]
The researchers studied biparametric MRI in 72 patients. All but three had “completely adequate and appropriate interpretations of their study,” he said, adding that the three cases failed because the men had hip replacements that interfered with MRI signals. “It doesn't really work if you have a hip replacement. If you have metal in your hips, then you have to get the contrast. And for men who've had HIFU or cryoablation or any other focal therapies, again, it doesn't really work as well, and you should still get contrast,” he said.
Pockros said these findings are critical for men who opted for AS for prostate cancer. He noted that MRIs are used in two ways in this population: in detecting prostate cancer and secondly, in deciding which men should undergo a biopsy, but also for monitoring prostate cancer in AS patients.
Pockros said the group did an economic analysis that found biparametric MRI was about $700 cheaper for men with commercial insurance, improving cost-effective prostate care.
He said the researchers will next analyze patient feedback on biparametric MRI to further refine prostate cancer imaging techniques.
(See more below. Now this for a developing story:)
Breaking story: Fewer men with Grade Group 1 cancer are opting for surgery
By Howard Wolinsky
A large study of two major patient registries—Surveillance, Epidemiology, and End Results (SEER) and Michigan Urological Surgery Improvement Collaborative—discovered that from 2010-2024 the proportion of patients found in post-prostatectomy biopsies to have Gleason 6/GradeGroup 1 had declined five-fold.
“These findings suggest that management of low-risk prostate cancer has improved during the past two decades, with a substantial decrease in the frequency of pathologic Grade Group 1 prostatectomies,” reported lead author Steven Moda, MD, a urologist at the University of Michigan (Go Blue!) and his colleagues.
The paper appeared in JAMA Network and was presented this week at the annual meeting of the American Urological Association in Las Vegas.
This cohort study included 185,928 patients who underwent radical prostatectomies from 2010 through 2024.
The proportion of radical prostatectomies resulting in GG1 on final pathology reports decreased from 32.4% to 7.8% between 2010 and 2020 in SEER and from 20.7% between 2012 and 2024 in MUSIC.
Researchers compared the proportion of Gleason 6 patients found in a population of 185,928 patients who had undergone radical prostatectomies.
Peter Carroll, MD, MPH, one of the pioneers of Active Surveillance in the 1990s, said: “Very good and timely article. Two things happened during this period: 1. Greater uptake of AS and 2. Urologists started not to biopsy based on PSA alone but increasingly used secondary serum and urine biomarkers (ie 4K etc.) and MRI before biopsy to better determine who was at risk of higher-grade disease and selectively biopsy those patients. Detection rates of GG1or unnecessary biopsy rates decreased. Both very good things.”
(More to come.)
Don’t miss the Active Surveillor’s free webinar with top urologist Dr. Jonathan Epstein on May 17
“What you need to know about your prostate biopsy--the new news”
Dr. Jonathan Epstein with Howard Wolinsky, editor, The Active Surveillor
Saturday, May 17 at Noon - 1.30 pm Eastern.
Register here
Hosted by The Active Surveillor with ASPI and AnCan Foundation
Join Dr. Jonathan Epstein (Ep-Stine) and Howard Wolinsky on Saturday May, 17. The program will focus on men on early Active Surveillance but also consider those contemplating or doing radiation therapy and surgery.
Dr. Jonathan Epstein recently launched Advanced Uropathology of New York (affiliated with Integrated Medical Professionals, PLLC) after nearly 40 years on the faculty at Johns Hopkins University School of Medicine.
(Dr. Jonathan Epstein)
If you have questions for Dr. Epstein, please send them to howard.wolinsky@gmail.com
A Medical Physicist’s POV on Biparametric MRI
By Howard Wolinsky
Gregory Karczmar, PhD, a medical physicist at the University of Chicago, has been challenging the myths of MRIs and advocating for MRI reform for years. He believes that Active Surveillance patients undergoing MRIs are getting more than they need: 3.5-Tesla machines when 1.5-Tesla will do the job—though it’s hard for patients to navigate these prostate imaging options.
He is a cancer survivor whose colorectal cancer was found on screening. So he is a strong advocate for cancer screening based on personal experience.
(Do we need a Tesla 3 and gadolinium for a prostate MRI? No.)
I asked him for his analysis of the University of Michigan study. Here’s what he said:
This study is super important and demonstrates the efficacy of Active Surveillance. Active Surveillance with MRI is vastly underutilized and is extremely beneficial for patients. It can cut back on the huge number of unnecessary biopsies, that cause a lot of discomfort, anxiety, and a fair number of adverse events in prostate cancer diagnostics.
For Active Surveillance, mpMRI is much better than standard PSA testing and DRE followed by 12-core biopsy. In fact, studies like this suggest that beyond Active Surveillance, mpMRI should be used in the general population for more extensive first-line prostate screening. As I probably mentioned to you in the past, our hybrid multidimensional MRI method is significantly better than mpMRI, so there are MRI innovations coming along that will make Active Surveillance and prostate screening even more effective.
(Gregory Karczmar, PhD, and his late best friend Madelaine, who died from cancer. Karzmar is a fan of screening. That’s how his own colorectal cancer was found.)
3. Although the hospital costs for MRI are very high, this doesn't represent the true costs, and especially the non-contrast scans that these authors are testing can be relatively inexpensive. One important point about non-contrast MRI—they can be done outside of hospitals with no physician present. This means costs are much lower. In addition, they can be done in the community, so that they are much more accessible, and men can come in for a 10-15 minute scan at lunch break. Then if there is something concerning on the biparametric scan, men can be sent to the medical center for more extensive prostate work-up.
When you consider all of the costs of unnecessary biopsies, costs of missed cancers that have to be treated at an advanced stage, loss of work time, and other financial and emotional damage to families and communities, MRI without contrast makes sense even though it is a bit on the expensive side. I think we can get the costs down to $400 or less for prostate MRI scans.
In the abstract, they don't mention what kind of scanner was used—but I would like to see some tests on a 1.5 T scanner or even lower field because these scanners are easier and much cheaper to site and operate and also much safer for operation outside of a hospital. I think a dedicated scanner for prostate cancer screening could be built with current technology that would make MRI screening cheaper—and also more effective than the scans done with current multi-purpose scanners. If we focus the design on pelvic exams, we can screen for prostate cancer effectively and efficiently, and in addition, these scanners could be used to screen for and diagnose other common conditions like uterine fibroids and uterine cancer.
The current structure of medical care for prostate cancer makes change difficult because there are turf battles, established procedures, financial interests of manufacturers, and other stakeholders. The medical establishment is really calcified. This makes change very difficult. But in my view, the scientific evidence—including the article you are reviewing—strongly supports the use of MRI for Active Surveillance and increased use of MRI for first-line prostate screening. The barriers at this point are more political, administrative, and logistical. I think public opinion and publications like yours can move things along a lot more quickly and significantly improve prostate cancer management and patient outcomes.
[He made some points on Dynamic Contrast-Enhanced Magnetic Resonance Imaging (DCE-MRI), a technique used in MRI to visualize and quantify the movement of a contrast agent within tissues. It provides information about tissue perfusion, permeability, and blood flow, making it valuable for diagnosing and evaluating various conditions, including brain tumors, multiple sclerosis, and prostate cancer.]
There is some evidence—including our own work—that suggests that for African American men, DCE-MRI is much more important for finding prostate cancer than for Caucasians. In fact, for African Americans and perhaps also for Africans, DCE-MRI may be the most effective screening method. So if this is true, this creates problems for methods (including our own) that are proposed for screening without contrast media injection. These findings have not yet been verified and are only speculative at this point. However, this could turn out to be a significant issue, since DCE-MRI scans have to be performed at hospitals and are much more expensive, and of course, there are concerns about long-term use of contrast agents.
Subscribe to my Substack for more cutting-edge insights on prostate cancer innovations, Active Surveillance strategies, and patient-centered care to stay informed and empowered in your prostate health journey!







I personally have no intention of having my P-gland removed under any foreseeable circumstance (I'm 71). Imaging is the key, and frankly, micro-U/S blows MRI out of the water on so many, many fronts. Yeah, there's the 'where it takes place' issue, but at some point you have to man-up and accept the inevitable. When (and if) my PCa get's noticeable, I will do focal of some sort. In the interim, and this is de rigeur for men on AS, diet+supplements to 1) shrink the gland (BPH) and 2) bolster the immune system. At some point, and it could be a decade or more off, a rogue cell might get loose and cause issues...then there is radiation and chemo, or just wait for a comorbidity to take me out. It's a continuing fight, Mother Nature has always favored her girls over us boys when it comes to longevity.
Interesting article regarding mpMRI (with contrast) vs. bpMRI (without contrast). I have had three MRIs total in the last five years. The first two were mpMRI, the my doc switched the third one to bpMRI. I was concerned about that, but he mentioned the bpMRI gives him all the information he needs. Now, I have another MRI to schedule for this coming October and he wants to switch back to mpMRI??? His reasoning was that he likes to use contrast "on every other MRI". Seems strange to me. I may just tell him I want the bp MRI again so as to avoid the contrast.