PCa Xmas miracle revisited--how 'Santa CDC' came down the chimney with $1 million gift to research Active Surveillance
Ho, Ho, Ho: Happy Xmas, Hanukkah, Kwanzaa, Super Solstice, Chelleh, Festivus
(Editor’s note: On December 23 two years ago, I got the word from the CDC that it was allocating $1 million for a major study on minority men and Active Surveillance issues. This was a first.
(Many of the important studies on AS were done outside the U.S. So this was considered a big deal.
(I had given a brief talk at a meeting of the American Society of Clinical Oncology early in 2023 where I mentioned the lack of research on views of Black men and Latinos regarding AS. A researcher from the Centers for Disease Control, who happened to be in the audience, contacted me a few days later and recruited me to help her develop a proposal for a study to be let out for bids. Drs. Matthew Cooperberg and Stacey Loeb won the bid and became principal investors on the study, which just got underway. I serve as an advisor. Below is a reprint of an article from Dec. 23, 2023.)
By Howard Wolinsky
(Santa CDC has a Coke and smile for AS-plus for $1 million study.)
Active Surveillance just got a $1 million and change gift for Kwanza, Xmas, and Hanukkah, ftom the federal government to research AS, especially hard-to reach Black and Latino men on AS.
(Hannukah Harry from SNL lit a candle for AS.)
The Centers for Disease Control and Prevention is following up--”refielding” in their words--a study I co-led with the late Herb Geller, Ph.D., an AnCan Foundation board member, and James Schraidt, an AnCan moderator and ZERO board member, that broke new ground on AS patients’ views on renaming Gleason 6 (Grade Group 1) as a non-cancer; what AS patients experienced with emotional distress, what AS patients thought about transperineal vs. transrectal biopsies. Other support groups and medical experts also pitched in. (See story below.)
More than 460 patients responded to our survey on SurveyMonkey in fall 2022.
In February 2023, I was invited by organizers to give a three-minute remote presentation on our findings at an off-site meeting at the American Society for Clinical Oncology in San Francisco.
I reported that only 5% of respondents said they would drop surveillance if Gleason 6 were renamed a non-cancer. That was big news because critics of the name-change worried that a large number of men would abandon surveillance and expose themselves to missing diagnoses and ending up with advanced and metastatic disease. (This phenomenon already was happening, based on 2023 figures from the American Cancer Society, without changing the designation of Gleason 6 prostate cancer.)
And 82% of respondents said they would stick with surveillance even with a name change. The remainder were undecided.
If Gleason 6 were redefined as noncancer, only 5% of patients say they would quit surveillance; 82% would stick with program.
·
February 16, 2023
I also published the survey as a letter in the Journal of the National Cancer Institute later: https://academic.oup.com/jnci/article/115/10/1236/7243176?login=false
During my talk, I pointed out a significant defect in our survey. I noted that only a handful of respondents were Black or Hispanic. The demographic profile of our respondents was lily-white, affluent, and highly educated--even though research shows AS is a viable option for minority men.
As it happens, a top prostate cancer researcher from the Centers for Disease Control and Prevention (CDC), Ingrid Hall, PhD, was in the audience. The CDC considers prostate cancer a major public health issue.
A few days after the event. on Feb. 28, Hall contacted me and recruited me to help in “refielding” our survey and “oversampling” Black and Hispanic patients.
“Would you be interested in discussing how CDC might be able to make that happen?” she asked me.
In a New York minute.
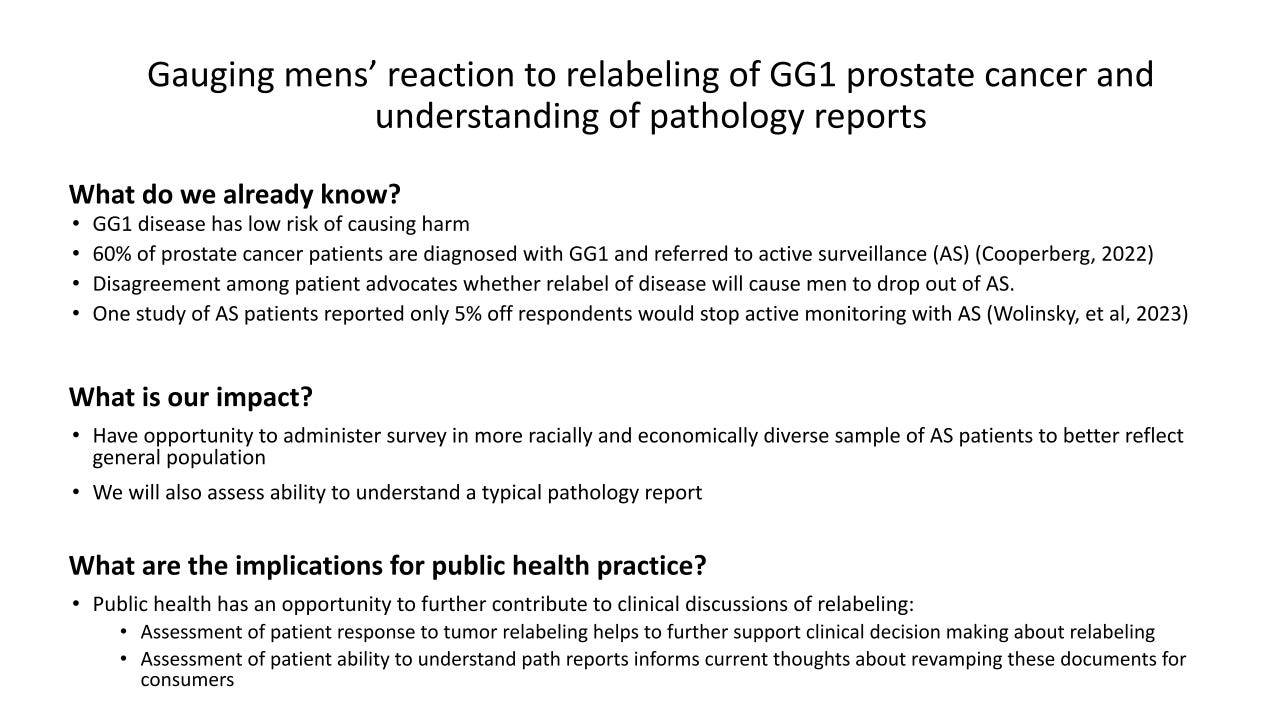
I met with Hall, a couple of times on Zoom and online to hone her presentation, developing this slide for her elevator pitch:
She warned me that it would be hard to get money for this because it required Congressional funding. But frankly, every step of the way, she told me how the proposal sailed through and now we’re cued up for a five-year, just over $1 million study.
Wow.
This may be among the largest AS studies to date--since the 800-pound gorillas in prostate cancer research, such as the (Advanced) Prostate Cancer Foundation and the U.S. Department of Defense’s Congressionally Mandated programs virtually ignore AS to focus on breakthrough drugs for the few men (about 3% of the PCa population) with advanced cancers vs. the 25% on AS with Gleason 6.
(Look on page 61 https://www.dropbox.com/t/KF1f8JbOwntBdeyB for the details.)
Stacy Loeb, MD, a urology and lifestyle medicine expert at NYU, and a columnist for this publication, said: “It is so rare to see funding opportunities related to active surveillance, so you should be very proud of making that happen! Congratulations on another victory of your advocacy to push forward the research on active surveillance!”
Here’s a summary: “The purpose of this project is to design, conduct, and analyze a study of patient perspectives on relabeling GG1 [AKA Gleason 6]as non-cancer, where respondents are a random sample of men with low-risk, localized prostate cancer from a population-based source (e.g., state cancer registries or equivalent), where the study would include sufficient numbers of African American and Hispanic men to provide reliable estimates about those groups, and would support analysis by race-ethnicity, socio-economic status (SES), insurance status, and social determinants of health.”
The research will focus on anxiety and emotional distress, an overlooked topic at the American Urological Association. See:
EXCLUSIVE! Read all about it: 'Deep Prostate' spills the beans on why AUA has no guideline for screening PCa patients for emotional distress
December 5, 2023
The CDC continues on to discuss anxiety and the need to rewrite pathology reports and relabel Gleason 6 as a noncancer: “The applicant will assess patient anxiety, degree of anxiety, and reasons why AS may have been discontinued among respondents. An additional purpose of this project is to design, conduct, and analyze a study of patient understanding of the wording about Gleason Grade Group 1 included on pathology reports, so that, if appropriate, the wording of pathology reports shared with patients (e.g., through patient portals) in the future can be improved to provide clinical context and be more patient-friendly. The results of this study will help inform the discussion about whether GG1 should be relabeled as non-cancer, and also may be useful in planning interventions to increase clinician use of active surveillance as the first choice of care for patients with GG1 prostate cancer.”
The project is out for bids. There is a possibility, as a graduate student in public health at the University of Illinois Chicago, I may be able to play a part. I could be the world’s oldest intern. Fingers crossed.
AS, long a prostate research pariah, the Rodney Dangerfield of research, which got no research respect, is finally finding a niche.
Here’s my ASCO talk:
Hi. I’m Howard Wolinsky.
I’m a Chicago-based medical journalist and a prostate cancer patient.
First, I’ll share my experience as a patient on AS--I celebrate my pros mitzvah this year--and then I’ll present broader views based on a survey of more than 450 patients about issues faced by patients on AS, including renaming Gleason Grade 1.
I experienced financial toxicity soon after I was diagnosed. Eight insurers considered me a bad risk for term-life insurance because I left untreated a single core of Gleason 6. I previously only had preferred insurance rates.
As a co-founder of support groups aimed at AS patients, I see and hear the emotional distress in the faces and voices of fellow low-risk patients. Some with Gleason 6 are driven to leave AS because they are going through anxious surveillance.
Renaming Gleason 6 as a non-cancer could help reduce the emotional distress and financial toxicity of low-risk patients like me.
I can share more than my opinion. Last fall,a coalition of support organizations, including ASPI, AnCan and Prostate Cancer Support Canada, and my newsletter, TheActiveSurveillor.com, along with some physician experts surveyed patients via SurveyMonkey. [Our poster was presented yesterday by Rick Davis, founder of AnCan, at the ASCO Genitourinary Congress.]
The Epstein 2 and other opponents of redefining Group 1 as a noncancer argue that patients will end surveillance if Gleason 6 were redefined as a noncancer.
But only 5% of respondents said they would quit surveillance. 82% said they would remain on AS. 13% were undecided.
The Eggener 6, led by Dr. Scott Eggener, my former urologist, of which I was the sole patient member, raised questions about Gleason 6 diagnoses causing financial toxicity. We only had anecdotal evidence.
16% of respondents said their insurance was canceled or their premiums jacked up because of a Gleason 6 diagnosis. Most had problems with term life followed by health insurance.
And there are issues with emotional distress from the diagnosis.
More than 90% said their urologists had not screened them for emotional distress even though ASCO, NCCN, and others recommend all cancer patients be screened. AUA and ASTRO guidelines don’t mention screening for emotional distress.
Patients are as divided as their doctors about a Gleason 6 name change.
We found 35% supported the name change, and the same proportion opposed it. The remaining 30% were undecided.
Affluent, well-educated white men responded to the survey. 19% had MDs, JDs and other advanced degrees.
Unfortunately, few Black and Hispanic men responded.
Are minority men not being offered AS?
Financial toxicity calls for a deeper analysis. How real is it and what can be done about it?
More research is needed on whether the name change will help retain patients on AS, overcoming the atrocious AS dropout rate from AS, 50% at five years and 66% at 10 years.
Need an AS pep talk? Check out my interview at GU Cast in Australia: https://www.gucast.org/episodes/we-meet-the-active-surveillor-howard-wolinsky’’
Have you heard about MRI-invisible lesions? They’re supposed to be good.
By Howard Wolinsky
Did you know that it’s possible for prostate cancer can spotted by a pathologist but the lesion can be invisible in an MRI?
Is this a good thing? Many researchers think it is a good thing.
Dr, Mark Emberton, Professor of interventional oncology at University College London and Dean of its Faculty of Medical Sciences, will be speaking to the ASPI webinar on Saturday, January 25, 2025, from noon – 1:30 p.m. Eastern (5:00pm-6:30pm UK time), about MRI-invisible lesions. Emberton is a pioneer on the use of MRIs in diagnosing, classifying and monitoring prostate cancer.
Don’t be invisible. Register here: https://zoom.us/meeting/register/tJYldu-qqzojGNEzCkgPQuTOWYGhcL80Dhec'
MRI-invisible lesionms are considered a good thing, comparable to Gleason 6.
Professor Emberton’s clinical research is aimed at improving the diagnostic and risk stratification tools and treatment strategies for prostate cancer (PCa). He specializes in the implementation of new imaging techniques, nanotechnologies, bio-engineering materials and non-invasive treatment approaches, such as high intensity focused ultrasound and photo-dynamic therapy.
His research has been published in over 300 peer-reviewed scientific papers in journals including BMJ, Lancet Oncology and European Urology. He has also contributed to the development of guidelines for the management of PCa and lower urinary tract symptoms, published by the International Society of Geriatric Oncology and the European Association of Urology.
If you have questions, please send them to: contactus@aspatients.org
An unsolicited endorsement for TheActiveSurveillor.com
Jim, You’ve been a miracle worker for ZERO as a board member and an AS moderator for AnCan—and more. It’s been an honor working with you. We’re kicking some ass now—better than kissing it.
Tick-tock. Do you want to attend the Jan. 4 AS year-in-review webinar, featuring four top prostate experts. You need a paid subscription, If you feel you can’t afford one, please contact me at Howard.wolinsky@gmail.com. I know a guy who can get you in.
Have you heard about MRI-invisible lesions? They’re supposed to be a good sign,
By Howard Wolinsky
Did you know that it’s possible for prostate cancer can spotted by a pathologist but the lesion can be invisible in an MRI?
Is this a good thing? Many researchers think it is a good thing.
Dr, Mark Emberton, Professor of interventional oncology at University College London and Dean of its Faculty of Medical Sciences, will be speaking to the ASPI webinar on Saturday, January 25, 2025, from noon – 1:30 p.m. Eastern (5:00pm-6:30pm UK time), about MRI-invisible lesions. Emberton is a pioneer on the use of MRIs in diagnosing, classifying and monitoring prostate cancer.
Don’t be invisible. Register here: https://zoom.us/meeting/register/tJYldu-qqzojGNEzCkgPQuTOWYGhcL80Dhec'
MRI-invisible lesionms are considered a good thing, comparable to Gleason 6.
Professor Emberton’s clinical research is aimed at improving the diagnostic and risk stratification tools and treatment strategies for prostate cancer (PCa). He specializes in the implementation of new imaging techniques, nanotechnologies, bio-engineering materials and non-invasive treatment approaches, such as high intensity focused ultrasound and photo-dynamic therapy.
His research has been published in over 300 peer-reviewed scientific papers in journals including BMJ, Lancet Oncology and European Urology. He has also contributed to the development of guidelines for the management of PCa and lower urinary tract symptoms, published by the International Society of Geriatric Oncology and the European Association of Urology.
If you have questions, please send them to: contactus@aspatients.org







Dr, Harley, Everyone is entitled to an opinion. The cancer vs. non-cancer does seem silly. But have you encountered anxious surveillance or SCANxiety? The hope is a redefinition will help men to not be diagnosed with a cancer to begin with. About 55% of this group of patients have emotional distress issue. And 10% of them feel so distressed that they seek aggressive. treatment and are placed at risk of incontinence, ED and even death. Have you run into financial issues because of the cancer diagnosis? 16% of us report having such issues as declined life insurance because we have "cancer." So you may blow this off as a non-issue but it is an issue for many of us. (Sources supplied upon request. Howard,
Having now been 'involved' with PCa for some time (starting with a prostatitis PSA scare in 2018) and currently 2 years into AS, I find the cancer/no-cancer debate somewhat ridiculous, a to-may-to/to-mah-to kind of thing.
At the end of the day, G6 and BPH are both 'cancers' in a sense, but since they are not malignant (able to metastasize), they are not Cancer with a capital 'C'.
Once a man presents with a prostate with other than normal prostatic tissues, he needs to be on AS at a minimum. Of course, just my opinion, doctor, but not medical 😉.