Past time for all PCa patients to undergo germline genetic testing. Let's spit for science and our health.
Brits: PCa surpasses BrCa. You read it here first.
By Howard Wolinsky
It’s well past time for us to stand up and spit for science.
Germline testing is considered standard of care for breast, ovarian, colorectal, pancreatic, and metastatic prostate cancer.
But unfortunately, even patients with metastatic prostate cancer and/or castration-resistant disease are not being tested routinely—with the cheap—even free—spit tests that can help them and their at-risk family members. The uptake in this population is only 4%-13% ,researchers are reporting. The numbers are even worse in non-White, rural, and economically disadvantaged populations.
And the uptake has been shown to be as low as 1%.
Germline testing can help determine your course of treatment and can flush out your at-risk family members.
This falls on our clinicians and the guideline-writing groups. It also falls on us patients.
Come on guys. I’ve been urging American patients for three years to undergo free testing in the Promise study from Johns Hopkins and the University of Washington. (Dr. Channing Paller, principal investigator from Hopkins, said there are no plans to extend the study to Canada.)
Check out my story. And go to the Promise study: prostatecancerpromise.org to sign up. Don’t wait.
And yes, I took the test myself. Click here to read all about it.
Leading researchers say it’s time that patients with low-risk prostate cancer get universal germline testing (UGT) and for groups that write guidelines to adopt universal testing as a standard and individual practitioners urge us to be tested.
Germline testing looks at actual inherited genes from our mothers and fathers as opposed to somatic testing, which reviews the tea leaves based on the genes produced by our cancers themselves. The presence of BrCA mutations, for example, is linked not only to breast cancer, ovarian cancer and pancreatic cancer but also prostate cancer, and can impact the course of treatment.
Read about Joel Axler’s genetic journey on Active Surveillance.
'Wildcard’: A journey of genetics, waiting, frustration, desperation, and, finally, a big decision
(Editor’s note: Joel Axler posed some serious issues for the moderators at the AnCan Virtual Active Surveillance Support Group. Axler, on the surface, appeared to have low-risk prostate cancer. But he had a plot twist—genetic mutations that doctors increasingly are taking seriously in finding a path to treat prostate cancer. Just how ‘active’ should hi…
We’re up the creek without a spit test. There are tests, like that from Color Diagnostics, that can do the job, but guidelines are not showing the way out of this mess.
Shockingly, the complexity of the current criteria impedes real-world adoption of prostate cancer GGT (germline genetic testing). “Accordingly, prostate cancer has one of the lowest rates of GGT utilization, with one contemporaneous study finding that only 1% of affected individuals underwent GGT,” Neal Shore, MD, and other leaders in genetic testing in the December issue of ASCO Oncology Practice.
(Neal Shore, MD, Medical Director, Carolina Urologic Research Center.)
Their article conveys a sense of urgency with the title: “Implementation of Universal Germline Genetic Testing Into Standard of Care for Patients With Prostate Cancer: The Time Is Now.”
What has happened up to now, as they say in Yiddish, is a “shanda,” a disgrace.
The researchers added “It is imperative that patients be offered timely and equitable access to testing as it can inform patient-physician shared decision making for management of the current cancer as well as anticipatory guidance for disease progression.”
They note that universal germline genetic testing “allows all patients with cancer, regardless of stage, pathology, or family history, to undergo GGT. The importance of universal GGT has been highlighted by several studies which have demonstrated that guideline-directed GGT may miss up to 55% of patients with actionable pathogenic germline variants.”
The shandas keep piling up.
Shpre & Co. said universal testing can not only help patients but their at-risk family members.
“A transition from guideline-directed to universal GGT has been recommended for breast, ovarian, and pancreatic cancer; however, universal testing has not yet been recommended for prostate cancer,” they noted.
Brian Helfand, MD, PhD, chief of urology at NorthShore University HealthSystem outside Chicago, a co-author of the paper and a speaker at “Active Surveillance 2025: The Year in Review” on Jan. 4, told me universal testing overcomes the spotty and unreliable information available from famikly histories.
]He said: “Family history information is the basis of guidelines for reimbursement for genetic testing. Family history is like a flip of a coin— as many patients don’t know this information, it changes over time, many patients don’t have a family large enough to come to conclusions, etc.”
He said to the AS 2025 forum: “It is not surprising that if you use current guidelines for genetic testing— [you] would miss 60% of men with mutations. As such, we don’t have a good bar to distinguish those who would benefit from those who wouldn’t. Now that genetic testing is affordable—all men should get it because there are so many important implications from screening to treatment that can be guided by this information
“[Discoveries in] 2024 has demonstrated that genetic testing, germline DNA testing for many of these type of genes should be had and should be expanded. The current NCCN [National Comprehensive Cancer Network] guidelines are relatively limited in terms of who is a candidate for getting germline genetic testing. Certainly, the cost has gone down, and so you can even, if you weren't covered by insurance, get these tests for relatively cheap in the order of about $200 these days.
“On the other hand, with the guideline expansion, more and more patients should be covered. And what I say that is that there's been a push based on a prospective trial, which was a national trial that demonstrated that only 60 percent of patients who met guideline criteria had gene mutations, but another 40 to 50 percent of men who had those mutations were actually based on the current NCCN guidelines would have not been offered testing. … ultimately, there's a push right now. And I think 2025 [will] see more universal or uniform germline genetic testing that's offered.”
(Note: Helfand is a urologist and a molecular biologist, the scientists who develop germline and other tests. He worked with GoPath Diagnostics to Buffalo Grove, Illinois. to develop ProstateNow, a germline test that assesses the risk of developing prostate cancer. Also, he’s my urologist.
(To view his talk and others at AS 2025, go here:
(After viewing the video, please respond to the survey: https://forms.gle/iww9y9gcj44Ei5PLA)
Shore, Helfand, et al. said their data supports “the notion that clinicians should offer all patients with prostate cancer the opportunity to undergo comprehensive GGT for pathogenic germline variants known to be associated with familial cancer and/or known to have implications for treatment and management.”
They said: “Democratization of GGT by universal testing is particularly relevant for patients with prostate cancer, for whom there are multiple and sometimes conflicting guidelines for GGT published by various professional societies and consensus committees. The National Comprehensive Cancer Network Prostate Cancer guidelines have recently removed pretest guidelines for GGT and clinicians are now directed to the Hereditary Breast, Ovarian, and Pancreatic and Hereditary Colorectal (Lynch syndrome) guidelines. This recommendation change could result in additional barriers to testing as prostate cancer clinicians will now have to navigate to a different set of guidelines of which they are most likely not routinely familiar.”
The researchers concluded: “Because GGT can inform patient-physician shared decision making, including therapeutic management, it is imperative that patients are offered timely and equitable access to GGT. Moreover, GGT is crucial for cascade testing of at-risk family members, identifying those who would benefit from risk-reducing interventions and enhanced screening to detect early-stage malignancies, including not only prostate but also breast, ovarian, pancreas, and colorectal cancers.
“Thus, we recommend that all patients with prostate cancer should be offered comprehensive GGT for assessment of PGVs in genes that are associated with hereditary cancer and have implications for evaluation and management.”
Unsolicited testimonial
I was pleased to get this email from George Gillespie, one of the founders of ASPI, who in late April will have been on AS for 25 years. Quite a record.
“It was good to see you (and others) at last month's webinar, as well as yesterday's. I also wanted to express to you (as I have previously done to [ASPI chair} Mark Lichty and [ASPI executive director] Bill Manning) that I believe ASPI has evolved into a very significant organization in the ‘cause’ of Active Surveillance. Your contributions especially, as journalist, commentator, moderator, etc., as regards to the webinars, and the ‘after-hours’ discussions, has raised the standard of these presentations to a truly professional level. Thank you for your continued contributions. … I have, just today, viewed your YouTube video ‘Active Surveillance ’25: The Year in Review’ and once again must thank you for putting together, and sharing, such an excellent presentation.
Very good to reconnect!”
George, Great to hear from you. Hope to see you again soon. And as I have said here before, flattery gets you everywhere, Howard.
Along these lines I was looking up something last week and discovered Google has declared me a “Public Figure.” I don’t know why.
No worries. So far I have avoided relentless media attention and invasive paparazzi. I do worry that the constant scrutiny can lead to feelings of vulnerability, anxiety, and paranoia, affecting their self-esteem and overall mental well-being.
Prostate Cancer #1 most common cancer in UK—US may follow soon
By Howard Wolinsky
The British press is filled with prostate cancer news.
This Olympic hero (Sir Chris Hoy), that rock star, (Sir Elton John, Sir Rod Stewart) this unknown farmer and his brother have been sharing their prostate cancer journeys with the public.
(“Candle in the Wind” Sir Elton)
(“Forever Young” Sir Rod)
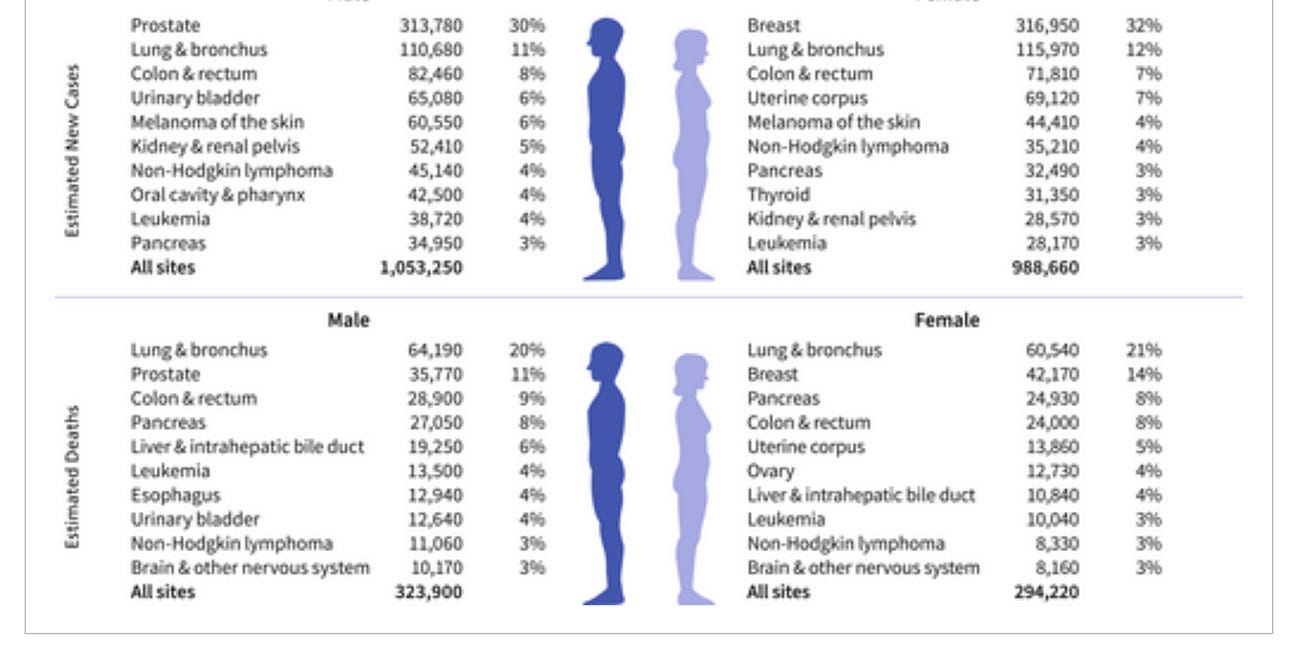
Now The Guardian is reporting that prostate cancer for the past two years has been Britain’s most common cancer, passing breast cancer in women: Prostate cancer becomes most common cancer diagnosis in England
The Daily Mail reported: Prostate cancer reaches the ‘grim milestone’ after high-profile cases including Sir Chris Hoy leads more men to get tested
It was front page news in the UK when Hoy, 48, cycling star and Britain’s most decorated Olympian with six gold medals in cycling, announced in February 2024 he has terminal prostate cancer that should have been detected early when treatable. The UK Health Minister responded by calling for a review of guidelines to urge more younger men to be screened. There are pushes on in UK to get more men screened and special programs to promote awareness and screening among Black men, who have double the incidence and death rates for prostate cancer.
When celebrities get diagnosed with cancer or other diseases, it’s an opening to promote changes in policies on detecting and treating those diseases. That’s why I carefgully follow these cases,
Readers of The Active Surveillor knew that already from stories in the past two years on how prostate cancer was the most common cancer in the UK. The Surveillor also reported recently that prostate cancer in the United States is on verge of passing breast cancer as the most common cancer. in a story covering how research funding on prostate cancer lags behind that on breast cancer in the U.S.
The Guardian reported, “There were 55,033 diagnoses of prostate cancer in England in 2023 compared with 47,526 diagnoses of breast cancer.”
The Guardian continued: “Prostate Cancer UK says the increase in diagnoses and awareness can be partly attributed to its awareness campaign launched with the NHS [National Health Service] in 2022, which has led to 3 million men using its online risk checker tool. More than 14,000 men who should have been diagnosed with the disease and referred to treatment were not due to the pandemic, but by April 2024 this gap had been closed.”
Try the Risk Checker here.
Chiara De Biase, director of health services, equity & improvement at Prostate Cancer UK, said the figures showed that prostate cancer awareness was growing across England.
I suspect if a similar campaign were conducted in the U.S. and other countries, the incidence and profile of prostate cancer would skyrocket. Maybe Congress, which includes several members with PCa, might get a fairer shake at funding.
The Cancer Surveillance Section at the International Agency for Research on Cancer (IARC), in Lyon, France, et al. reported:
“Prostate cancer is the most frequently diagnosed cancer among men in almost two thirds (118 of 185) of the world’s countries. Incidence varies markedly by region, and rates range from 6.4 to 82.8 per 100,000, with the highest rates seen in Northern Europe, Australia/New Zealand, the Caribbean, and Northern America and the lowest rates seen in several Asian and African regions. The regional patterns of mortality rates do not follow those of incidence, with the highest mortality rates found in the Caribbean and sub-Saharan Africa, indicative of disparities in early detection and treatment.”
The Lancet Commission on Prostate Pancer recently predicted a doubling worldwide of prostate cancer cases by 2040 and an 85% increase in deaths as I reported last year in Medscape. A tsunami is coming.
Prof. Peter Johnson, NHS national clinical director for cancer, said: “We know that coming forward for prostate checks can be daunting, but it could save your life, so we would encourage men to consult the prostate cancer symptoms advice available on NHS.uk, and to see their GP as soon as possible if they are concerned.”
The same advice applies worldwide.
ASPI about to close nominations for its 2025 awards program
Active Surveillance Patients International (ASPI) is inviting the surveillance community to submit ideas for its fourth 2025 awards program.
The awards program includes the Chodak Award honoring the late Dr. Gerry Chodak, ASPI’s first medical advisor and a University of Chicago researcher who encouraged the development of early conservative approaches to prostate cancer.
Winners have included such pioneers as Dr. Laurence Klotz, of the University of Toronto, Dr.Peter Albertsen, of the University of Connecticut, and Dr. Peter Carroll, of the University of California, San Francisco. All were early advocates and researchers of the protocol now known as Active Surveillance.
(For videos on all awards presentations, go to: https://aspatients.org/awards/)
Two other awards are now presented:
--The ASPI Special Awards to groups or individuals who have made major contributions to AS research. Winners have included Drs. Freddie Hamdy and Jenny Donovan, who were the principal investigators of the landmark ProtecT trial, which proved the safety and effectiveness of AS, and the Michigan Urological Surgery Improvement Collaborative (MUSIC) for its success in demonstrating how AS can be widely accepted in small or large practices in the community or academic urology practices, alike.
--The ASPI Patient Advocacy Award is named for ASPI co-founder Thrainn Thorvaldsson, the first recipient, and E. Michael Scott, founder of Prostate Cancer International, an early advocate for AS even though he doesn’t have prostate cancer.
“If you have names of folks who have fought the headwinds, and showed courage in furthering AS, please send them to us with your justification,” said Mark Lichty, ASPI chairman and co-founder.
Send your nominations to contactus@aspatients.org by Jan. 31, 2025.
European Association of Urology.
If you have questions, please send them to: contactus@aspatients.org