Part II: Fear and loathing on the road to PCa and Active Surveillance
The MRI era into the future
(Note: I have divided up my article on my AS-Quinceañero—15 years years on Active Surveillance for low-risk prostate cancer—into two pieces. I’m looking at what’s changed in 15 years and where things are headed. There have been so many changes—for the better. For part I, go to here.—HW)
By Howard Wolinsky
Multiparametric MRI (mpMRI) has been a game changer, but as usual the uptake of new technology such as MRIs to find high-risk cancers while avoiding biopsies has lagged in the U.S. compared to Europe.
A biopsy today is necessary to diagnose a cancer. But is diagnosing low-risk cancer really necessary?
The whole approach to MRIs, back when I had my first in 2011, was ass-backwards. Insurance companies, often the invisible hand in medical decisions, drove this. Back then, insurers wouldn’t pay for the procedure unless you already had had a biopsy confirming the presence of cancer. So it was the era of biopsies first.
That’s changed of course.
Prebiopsy MRIs
Prebiopsy MRIs are common in the U.K., helping men avoid unnecessary biopsies and unnecessary diagnoses. A leading urologist in the U.K., Dr. Mark Emberton, once told me the diagnostic process stops in practice if no cancer is found on a prebiopsy MRI. Not so in the Land of the Free and Home of the Brave. More here.
Prebiopsy MRIs are recommended in the U.S., but they are not widely used here yet.
Peter Carroll, MD, MPH, an AS pioneer at UCSF, told a meeting of Active Surveillance Patients International on Sept. 28. that he thought it was “ridiculous” that so many men going for biopsy without first undergoing a prebiopsy MRI.
Confirmatory biopsies?
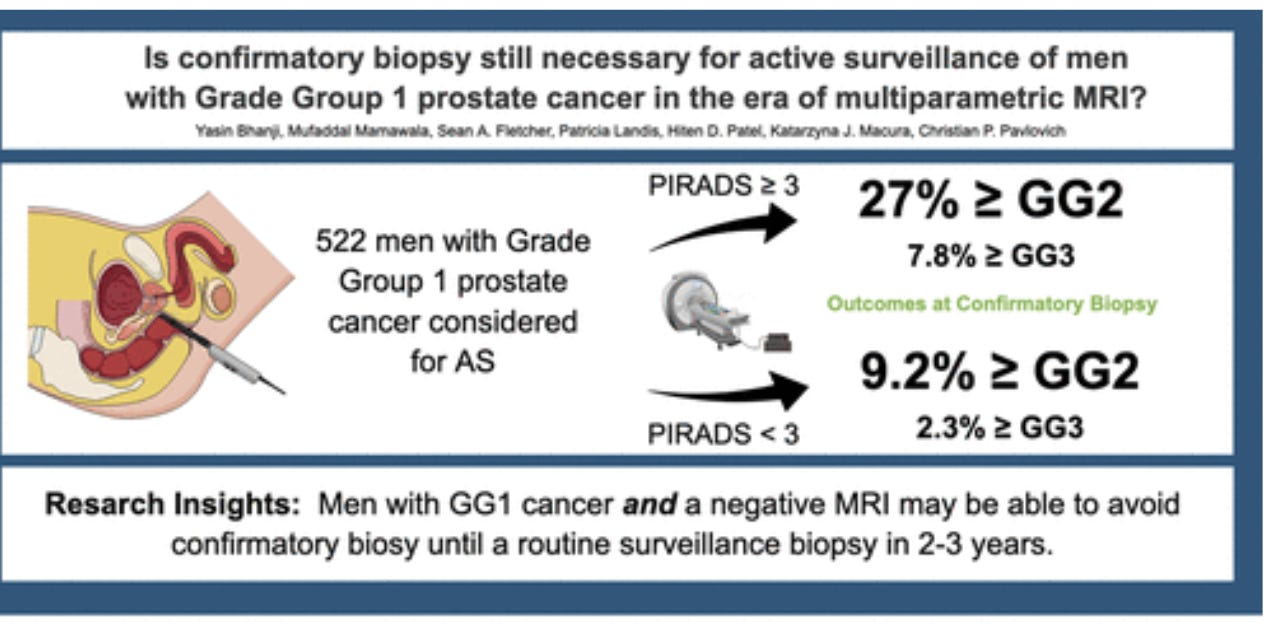
Another angle: MRIs are starting to displace confirmatory biopsies.
A confirmatory prostate biopsy is a repeat biopsy performed after an initial biopsy that diagnosed low-risk prostate cancer. This repeat biopsy helps determine if the initial diagnosis was accurate in identifying the extent and aggressiveness of the cancer, or if a more advanced tumor was potentially missed. It's done—usually a year to 18 months after the initial biopsy—particularly if the patient is considering Active Surveillance.
But Dr. Matthew Cooperberg, of UCSF, and his team showed that an MRI could replace a confirmatory biopsy for men diagnosed with Gleason 6 (Grade Group 1) cancer but not in men with favorable Gleason 3+4 (Grade Group 2) intermediate-risk cancer.
And “Hopkins researchers came to a similar conclusion: Confirmatory biopsies can be deferred in men diagnosed with low-risk PCa considering AS but who have negative MRI scans.”
Quick note: MRIs can contradict the cancer findings from biopsies. Many MRI lesions are “invisible,” which some urology leaders, including Dr. Laurenve Klotz, the AS pioneer at the University of Toronto.
Klotz and Emberton, of University College London, consider this seeming contradiction a positive sign though many U.S. doctors don’t seem to mention it.
Homing in on PCa with targeted biopsies
Targeted prostate biopsies have been another game changer. For years, critics ridiculed systematic biopsies as “blind” or “random,” “shots in the dark,” because they were imprecise though they followed a pattern to try cover the territory.
Now, with advanced imaging, like MRIs, fusion-guided biopsies can home in on suspicious areas. Fusion biopsies are about precise targeting of the cancer.
A fusion biopsy, also known as MRI-ultrasound fusion-guided biopsy, is a specialized prostate biopsy technique combining—fusing—MRI and ultrasound images to create a detailed 3-D model of the prostate. This allows doctors to target suspicious areas more precisely for biopsy, potentially improving cancer detection rates.
Fusion biopsies are generally available in academic centers. But sources tell me only 15% or so of biopsies are performed in these centers. The remaining 85% of biopsies are performed in community settings, often without a fusion technique available.
I never had a targeted biopsy—because no cancer has been found in my prostate in the “MRI era” that could be targeted.
An aside: Giving the finger to DREs
The so-called “finger wave,” the Digital Rectal Exam (DRE), 15 years ago was standard in prostate exams. Neither doctor or patient liked them. In fact, DREs were a deal breaker for many men, especially Black men, who had a cultural resistance to what some consider a homosexual act.
(I shot a photo in 2017 of my own urologist, Dr. Brian Helfand, gloving up for my last, DRE.)
In olden times, DREs detected advanced cancers. A DRE detected former President Joe Biden’s Gleason 9 cancer. This is unusual in the age of MRIs. Biden, 82, stopped PSA testing when he was 75.
But in general DREs are becoming a lost art. I served on a consensus panel for Movember, the major men’s health organization, that called for an end to DREs.
Check my article: Bye-bye 'finger wave'? More MRIs before biopsies? Movember consensus recommends sweeping changes to AS protocols: U.S. community AS practice lags a decade behind UK and US academic practice.”
Biden’s experience may lead some patients and urologists back to DREs, just to be safe.
‘Bug’ ? Or ‘feature’?
Not that MRI prostate scans are perfect; MRs miss about 25% of cancers,
One MRI bug works to the advantage of low-risk patients: Without a contrast agent, MRI is not great at finding low-risk cases, which make up the majority of prostate cancers. But even without contrast, MRIs an find the more advanced cancers that need attention.
What about skipping the contrast since MRI can locate threatening prostate cancers without it?
There is a move away from the common multiparametric MRI (mpMRI) of the prostate. In its place, some doctors are advocating biparametric MRIs (bpMRI).
BpMRIs streamline the process. They cut out the need for contrast, which saves both time and money, and relieves fears about side effects from the contrast agent, gadolinium.
Multiparametric biopsies require 45-60 minutes in the MRI tube, housing the superconducting magnets. The closed space of the tube can trigger claustrophobia in up to 15% of us, including me. Many more get anxious inside the tube while wondering what awaits them on the other side.
Back in 2011, I was among the first patients to undergo prostate mpMRI imaging. See “MRI shines a light on whether we need biopsies.”
MRIs have played an increasingly important role on the prostate cancer scene since benefits of mpMRIs and targeted mpMRIs, were proven 2018 in “PRECISION delivers on the PROMIS of mpMRI in early detection” in Nature MRI-”Targeted or Standard Biopsy for Prostate-Cancer Diagnosis” in New England Journal of Medicine. Also see “Lifting the 'burden of AS' with prebiopsy MRIs & biomarkers to avoid unnecessary biopsies, diagnoses, treatment.”
Gadolinium is the contrast used in mpMRIs. It is a potentially toxic chemical that can cross the blood-brain barrier
Some patients and some class-action lawyers began raising safety issues about gad in recent years: “Gadzooks! And Egads! Another Dilemma in Prostate Cancer.” You don’t hear much about this lately, but there are lingering concerns.
Radiology has reduced doses of expensive gad and is working on other potential solutions, including parametric MRIs.
Cutting out the contrast
Some centers now, such as the University of Michigan are using biparametric biopsies that take roughly 15 minutes--probably reducing risk for claustrophobia—and producing imaging sufficient to detect more advanced cancers while ignoring the low-risk ones. See The Active Surveillor: “Look mom--no gadolinium. And no more claustrophobia? New approaches coming to improve Active Surveillance experience”.
The Wolverine radiologists and urologists pretty much have eliminated mpMRI for prostate cancer diagnosis in Ann Arbor. Go, Blue!
Some experts think two-step prebiopsy biparametric MRIs hold the future at least in the intermediate term in screening. Some envision the adoption of prostate-specific MRIs to find more advanced cancers.
I underwent a biparametric MRI today. It was a breeze—though it took a bit longer than the ones in Ann Arbor—35 minutes. I got some very interesting results unofficially. I’ll share the them once I speak with my urologist.
Getting off the AS train?
I have been contemplating jumping off the AS train for a couple of years--though several experts recommend I have one last MRI before I make any final decision on AS.
I’ll soon to 78. Should I stay or should I go? I’m still thinking about it leaving behind AS.
Another change: Micro-ultrasound
I have been writing about the potential of micro-ultrasound for years.
I considered it as an alternative to mpMRI, though my doctor was reluctant.
However, new research has shown micro-ultrasound produced results equivalent to that of MRIs. See:
Plus, micro-US is a far cheaper approach and is covered by Medicare.
Amazingly, in Chicago’s vast Medical Mecca, micro-ultrasound is not available. I’d have to go to Indiana or Ohio to get one. I suspect hospitals in the Second City have opposed the office procedure to help cover overhead on their hungry MRI machines.
Future is bright
Many changes have been working in the favor of low-risk patients over the past 15 years.
We’re hearing good things about new biomarker tests that claim to outperform the PSA, such MyProstateScore 2.0 and a new test in Britain, both urine tests. There are many more tests such as blood-based Stockholm 3 and IsoPSA.
More accurate screening is long overdue with the high false-positive rate with PSAs. Seventy-five percent of men with high PSA scores do not have cancer.
Maybe we’ll see in the near future wider use of PSMA (prostate-specific membrane antigen) PET imaging. Right now, this is a tool for patients with Gleason 7—though I know some Gleason 6 patients who have managed to get them. The cost is high—about $7k in Chicago—but maybe cost can be brought down in the long-term?
PSMA can tell patient whether the cancer is contained in the prostate cancer capsule.
I suspect it has unfulfilled potential for Gleason 6 patients. Knowing the cancer has not moved into dangerous territory could help patients go on and stay on surveillance and maybe reduce or avoid emotional distress.
Genes
There were no commonly available genetic tests for prostate cancer when I started my cancer “journey.” It is widely available now, and it can help determine the intensity and course of treatment and flush out family members who are at risk and not only for prostate cancer. It’s time to spit for science.
I think genetic testing will play an even bigger future role as researchers understand more about which mutations matter.
See:
The evolution of AS
Many top urologic oncologists have told me that these days, if I were just starting out, I likely would not have been diagnosed with prostate cancer. I wouldn’t have gone farther than a prebiopsy MRI or a micro-ultrasound exam.
I would have just led my life as a freelance journalist and photographer.
But then, I wouldn’t have met so many nice people with low-risk prostate cancer in support groups I started or have started this newsletter—The Active Surveillor: Saving Prostates Daily—for patients like me and their spouses and families.
Some urologists now stress they don’t want to diagnose Gleason 6 cases.
The horizon
What else is on the horizon?
Urologists need to better define who should go on AS. Men with low-risk men should not be given tickets for the AS Express to begin with. Some places such as UCSF haven’t diagnosed very low-risk PCa in years.
On the other hand, the 40% of men with who opt for aggressive treatment need better guidance and education. They need screening for emotional distress—not endorsed in guidelines from the American Urological Association or American Society for Clinical Oncology.
I suspect there will be new paths coming for men with lower risk PCa who psychologically can’t live with “wimpy” cancers that will never kill them but are not screened for or helped for emotional distress like anxiety.
Likewise, maybe there will be more help for patients with high-volume Gleason 6 who opt to be treated, some of whom go on AS and others don’t depending on the philosophy of their urologists.
It may not quite be AS but immunotherapy such as Provenge or meds like “enza” may be options. Likewise, focal therapy has been gaining traction as a middle, less invasive path between AS and surgery and radiation.
Focal therapy, using various energies like heat and cold to remove prostate cancers rather than removal of the whole gland, seems to be gaining acceptance by an increasing number of urologists.
These treatments don’t meet the current definition AS. I’ve been told that I’m too literal in my definition of AS. A purist. But things are evolving. These middle-path approaches could still potentially save men from surgery or radiation.
Will the definition of AS be broadened to include modalities that are more invasive? Maybe.
Top leaders in the field have stressed they are not concerned about Gleason 6 patients and think that the future of AS will be for men with Gleason 3+4—only about 20% of whom go on surveillance now thought it’s 45% in the famed MUSIC program in Michigan—and shockingly in today’s approach, as I heard recently from UCSF’s Cooperberg, even Gleason 4+3 patients, some of whose cancers don’t seem to progress.
Long-term prostate biopsies may fade away as MRI and micro-ultrasound technology and AI advance. UCSF’s Carroll, the AS pioneer, told a webinar I organized that he tells young doctors mulling over their specialties to think twice about going into pathology or radiology because he thinks AI will take over—though uropathologist Jonathan Epstein is skeptical. I’d like to see AI capture Dr. Epstein’s world-class mental database to improve the technology.
Way out there is the idea of using proxy prostate cells made from stem cells and put in a dish to not only replace traditional biopsies but to test meds. Talk about personalized medicine.
My Quinceañero
As I observe my Quinceañero year, I’m hoping for good outcomes for our sons and their sons and coming generations as prostate cancer screening evolves and fewer of us are diagnosed with a so-called cancer that doesn’t need to be treated.
Diagnosing and treating prostate cancer is a vastly different enterprise than when I set out 15 years ago. The future is bright--gotta wear shades, as Timbuk3 put it:
July webinar: 'Why All Men Diagnosed with Prostate Cancer Should Undergo Germline Genetic Testing'
ASPI (Active Surveillance Patients International) has assembled a panel of genetics experts to address genetic and prostate cancer.
The session will run from noon to 1:30 pm Eastern time on Saturday, July 26.
Please register for the meeting here.
There will be a Question-and-Answer session following remarks by the panel. Please send questions in advance to: contactus@aspatients.org
Please respond to my confidential survey on genetic testing and PCa. Click here: https://forms.gle/Uv9d5gaZYHadZ5Qh9
Also:
lease answer this questionnaire.on transperineal vs. transrectal biopsies: https://forms.gle/GShpHwegEPtAVgTs9 I have a relevant story coming, and you can take a few minutes and help if you haven’t already.








Well done article. The underlying thread that I saw was the sad inability of a large number of men to 'man-up'. Unfortunately, this was the factor that had many Uros doing TRUS without any numbing to the prostate at all. Ya just can't win.
Thanks, Harley. I have not seen much of Facebook groups. I stopped looking when some guys referred to AS as "slow-motion suicide." I think they meant you were doomed unless you had a radical prostatectomy or aggressive radiation therapy. Is it still like that? Sounds like fear of AS. Not trusting it. And maybe rationalizing the decision to treat and maybe anger over side effects? What do you think?